|
Aging and Long-Term Care (10 Hours) > Chapter 2, Part B
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Chapter 2 Part 2: Biological (Physical)
Other Diseases of the BodyRheumatic DiseasesRheumatic diseases are "disorders of connective tissue, especially the joints and related structures, characterized by inflammation, degeneration, or metabolic derangement" (MDO n.d.). There are over 100 rheumatic diseases, many of which have historically been lumped under the term rheumatism. The discussion here is limited to those that most commonly occur to people age sixty or older, although they may also occur at other ages. OsteoarthritisOsteoarthritis is the most common type of arthritis---70% of those over seventy years old have x-ray evidence of this malady (Srikulmontree 2008). Osteoarthritis chiefly affects the tissue, known as cartilage, which pads the ends of bones within a joint. Osteoarthritis takes place when cartilage begins to wear or fray, sometimes completely wearing away, leaving a bone-on-bone joint (NIAMS n.d.a). [QN.No.#11.The most common type of arthritis found in elderly persons:] Some predispositions to osteoarthritis are:

Osteoarthritis may also cause disability which usually happens when the spine, knees, or hips are affected. Treatments for osteoarthritis are fourfold:
OsteoporosisOsteoporosis is a disease manifested by a decrease in bone strength; this leads to a greater risk of fractures, or broken bones (NIAMS n.d.b, 1). Osteoporosis is the primary underlying cause of fractures in postmenopausal women and the elderly. Bones of the hip, spine, and wrist more frequently sustain fractures, but any bone can be affected. Some fractures can be permanently crippling, especially if they are in the hip. [QN.No.#12.The primary underlying cause of fractures in postmenopausal women and the elderly is:] 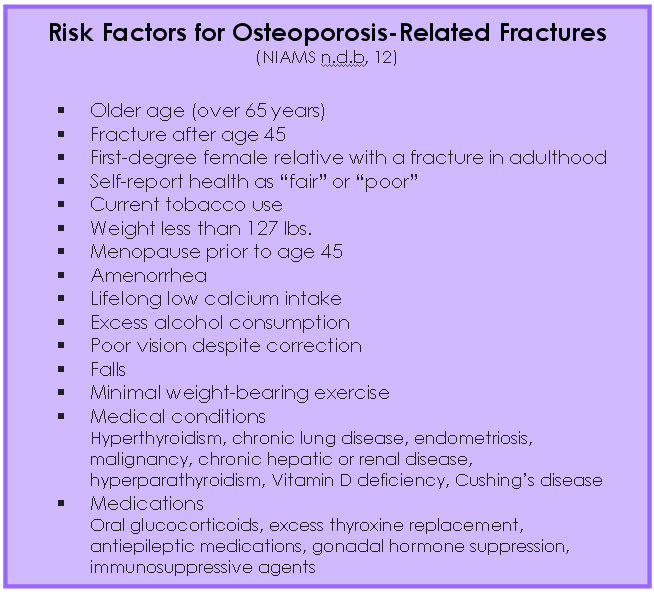 The first plan of attack is to aid your clients in preventing osteoporosis. The following are some of the ways an individual can help prevent and/or treat osteoporosis (NIAMS n.d.b, 17ff, 32ff):
Pseudogout Calcium Phosphate Crystals One of the risk factors of pseudogout is older age (Mayo 2008), whereas that is not as true of gout (Mayo 2007). Other risk factors of pseudogout are:
Polymyalgia RheumaticaAn inflammatory disorder, polymyalgia rheumatica (PMR) causes widespread muscle pain and stiffness, especially in one's neck, shoulders, upper arms, thighs, and hips. Symptoms may appear gradually or very suddenly. The exact cause of PMR is not known, but it is possibly a problem with the immune system; it may involve both genetic and environmental aspects. There may also be a link with particular viruses (Mayo 2008a):
PMR is diagnosed through blood tests: sed rate, rheumatoid factor (RF), C-reactive protein, and other blood tests. Polymyalgia rheumatica will usually resolve itself in one to two years, but symptoms may be improved with medications and self-care strategies. [QN.No.#13.An inflammatory disorder that is diagnosed through blood tests: sed rate, rheumatoid factor (RF), C-reactive protein is:] Symptoms may include:
Risk factors that may increase the likelihood of an individual getting PMR are (Mayo 2008a):
Doctors may treat the disease with nonsteroidal anti-inflammatory drugs (NSAIDs) or oral corticosteroid drugs such as prednisone, but they prefer not to use either of these medications over a long period of time because of potential side effects. Other things clients can do to help are:
About seven out of one thousand of those over 50 have PMR (WD n.d.), and anywhere from 15-25% of those also have Giant Cell Arteritis (GCA) (Werner 2008), another rheumatic disease. Because of its relatively small percent of incidence, GCA will not be discussed in this course, but healthcare workers are urged to learn more about it "just in case." Paget's Disease of BoneBones, as other parts of the body, continually rebuild themselves. When this happens at an accelerated rate, the bones can become misshapen and soft, a condition called Paget's disease of bone. If a bone has become soft through this condition, it can cause the involved pelvis, spine, hips, thighs, head, or arms to bend and be weak. If the bone is misshapen or enlarged, it is prone to arthritis and fractures and may cause hearing loss and discomfort (Altman 2006). [QN.No.#14.When bones rebuild themselves at an accelerated rate, the bones can become misshapen and soft, this condition is called :] This is a condition that is seldom diagnosed before age forty, and the frequency of diagnosis increases in each progressive age group to 10% by age 80 (WD n.d.a). For this reason, the symptoms are often assumed to be simply part of the aging process. Fortunately, the condition does not spread from bone to bone and is usually limited to one or a few bones of the pelvis, spine, hips, thighs, head, or arms (Altman 2006). Very rarely, in less than 1% of those with Paget's, it can lead to cancer---osteosarcoma---although this usually happens only after the individual has had Paget's for a long time. Osteoarthritis and congestive heart failure are more common complications of Paget's disease (Mayo 2008b). The only known risk factors are age and heredity, although men are more likely to get Paget's than are women. It is diagnosed through an alkaline phosphatase blood test, an x-ray---usually taken for unrelated reasons, and/or a bone scan. [QN.No.#15.The only known risk factor for Paget's disease of bone are:] [QN.No.#16.'Men are more likely to get Paget's than are women' . true or false] Symptoms, if any, will depend on the part of the skeletal system that is involved, and can include (Mayo 2008b):
One of two kinds of bone-regulating medications, bisphosphonates and calcitonin, may be prescribed. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin may be prescribed for inflammation, and acetaminophen (e.g., Tylenol) may be used to reduce pain. In a very few cases, the patient may need surgery to aid in the healing of fractures, to replace damaged joints, to realign deformed bones, or to reduce pressure on nerves (Mayo 2008c). [QN.No.#17. The prescribed bone-regulating medications are:] In addition to the anticipated healthy diet and exercise, Paget's patients need to take extra care to avoid falls. Diabetes MellitusAlmost twenty-four million Americans are estimated to have diabetes mellitus (ADA n.d.), and more than half of those are over sixty years of age. Of folks over age sixty-five, almost 20% have diabetes (NDIC 2002).
There are two types of diabetes (Mayo 2009; Inzucchi et al 2007a; Inzucchi et al 2007b):
As a person ages, insulin production tends to decrease because of age-related cell damage (including in the pancreas) causing a reduction of insulin output. Other tissues tend to become less sensitive to insulin. The risk factors for diabetes include (Mayo 2009):
[QN.No.#18. Which of the following is NOT a risk factor for diabetes?] It is most important that your clients be aware of potential symptoms of diabetes (Mayo 2009):
The physician may use one or more of the following tests to diagnoses diabetes (Mayo 2009):
As with most classes of diseases, there is some commonality between treatments but specific types of the disease may have special prescriptions and/or regimens. And, as with most of the diseases discussed in this program, for any type of diabetes a healthy diet and exercise should be considered part of the treatment plan. Additionally, someone with diabetes basically needs to monitor their blood sugar and to take insulin as prescribed. IncontinenceIn the elderly population, incontinence is a potentially disabling condition that is both common and disruptive. It is defined as the involuntary loss of urine or stool in an amount large enough to be a social and/or health problem (Kane et al 2004, 173). Urinary incontinence (UI), much more common than stool incontinence, affects 8-34% of the non-institutionalized elderly population (Merck n.d.) and 50-84% of the geriatric population in long-term care facilities (Ogundele et al 2006).
Urinary incontinence is a medical condition with numerous possible causes, but it is not a normal part of aging or, in women, an inevitable consequence of childbirth or change after menopause. It can result in lifestyle changes---changes in activities, work life, social and personal life---and in skin problems and urinary tract infections (Mayo 2007a). There are several kinds of urinary incontinence (Mayo 2007a):
There are six types of incontinence with their own symptoms (Mayo 2007a): 
Procedures that have a good chance of preventing urinary incontinence are:
There are a number of treatments for UI, depending on the kind of incontinence the individual has, the severity of the problem, and the fundamental cause of the problem (Mayo 2007a).
[QN.No.#19. Treatments technique which is usually used only for people with severe urinary incontinence who have been unable to respond to behavioral techniques or medications:] Many people do not tell their doctors about the urinary incontinence. They may be "used to it" and assume it is a necessary part of aging, or they may be embarrassed. You will need to be on the lookout for signs---verbal or otherwise---of UI, or you may need to ask in order to help your client find the best resolution to this problem. Chronic Obstructive Pulmonary Disease (COPD)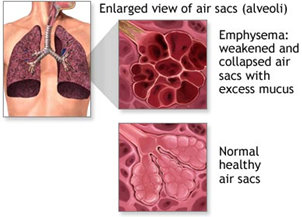 However, COPD is now considered a disease of a multisystemic nature, not just limited to the lungs. Research has found elevated Picture courtesy of A.D.A.M. degrees of systemic inflammation and cardiovascular, neurologic, psychiatric, endocrine system dysfunction, and skeletal muscle dysfunction associated with COPD (Stone and Nici 2007). Chronic obstructive pulmonary disease is the fourth-leading cause of death in the United States (NHLBI 2009). In most cases, long-term smoking is the cause of COPD. Not smoking or quitting smoking soon enough could prevent COPD. Unfortunately, once symptoms arise, the lung damage cannot be reversed. There is no cure. The primary focus of treatments for COPD is to control symptoms and prevent further damage (Mayo 2007b). The lowest percentage (8.8%) of adults that currently smoke is the elderly, folks age 65 and over (Nazir et al 2007). [QN.No.#20. Which disease is the fourth-leading cause of death in the United States:] However, the mean inpatient, outpatient, and pharmacy costs of patients aged 65+ who have COPD are more than twice those of age- and gender-matched control subjects who do not have COPD (Mapel et al 2000). Risk factors for COPD are (Nazir et al 2007):
Treatment for COPD includes (Nazir et al 2007):
For a client that resists quitting smoking, you might try the "5 R's" (PHS 2000; Radin and Cote 2008):
Counseling is generally recommended to help a client stop smoking (Radin and Cote 2008). The success for someone trying to stop smoking with no counseling is 13%, whereas intensive counseling has a 22% success rate. Most insurance companies now reimburse for smoking-cessation counseling visits. There are two types of counseling that seem to be most helpful in smoking cessation: cognitive and behavioral. Cognitive counseling aids clients to reframe the way they think about smoking by using distraction, positivism, relaxation, and mental imagery, as well as offered encouragement and motivation. Behavioral counseling helps smokers recognize and avoid particular smoking trigger stimuli:
There is a powerful correlation between the intensity and duration of the counseling and its effectiveness. Professionally led group counseling sessions are more effective than self-help, and often more than individual counseling. The best choice, however, is a combination of individual and group counseling. It is also essential that there be continuous social support from spouses, friends, coworkers, and professionals such as the physician or yourself. Tips for patients trying to quit smoking:
Although stopping or decreasing the amount of smoking will not promote recovery of lost lung function, it does reduce the rate of decline in the ratio Forced Expiratory Volume (FEV) (the amount of air that a person can forcibly blow out in one second, measured in liters) to Forced Vital Capacity (FVC) (the total amount of air that can forcibly be blown out after full inspiration, measured in liters). 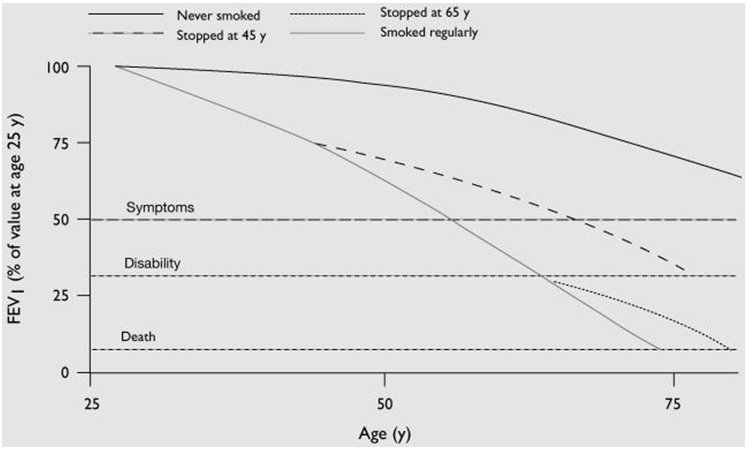 Changes in lung function after age 25 in smokers, nonsmokers, and ex-smokers, based on FEV1 (forced expiratory volume in 1 second). (Doherty and Briggs 2004) "Early diagnosis by spirometry is essential since patients at risk may dismiss telltale symptoms as the normal consequences of smoking. Prompt initiation of smoking cessation therapy can help improve airflow, partially reverse impaired lung function, slow the accelerated annual decline of FEV1 caused by tobacco smoke, and reduce the premature morbidity and mortality associated with COPD and other tobacco-related diseases. Initiation of appropriate interventions earlier rather than later, especially bronchodilator therapy, can improve symptoms, quality of life, and exercise capacity while decreasing the acute exacerbation rate and perhaps help to slow the progressive accelerated decline in lung function at minimal cost" (Doherty and Briggs 2004). Oncology in the AgingThe most important risk factor for cancer is aging. The occurrence of common malignancies increases with age; more than 60% of all carcinomas occur in those aged 65 or older and is expected to increase to 70% by 2030 (Balducci and Beghé 2008).
The death rate for surgery and the risk of other complications increase with age; however, even in patients older than eighty, elective surgery seems to be generally safe. The elderly from age 70 on do, however, seem to be greatly more susceptible to complications of emergency surgery, especially those related to the digestive tract. Therefore, a regular screening for colorectal cancer may reduce the need for emergency surgery. Recent advances in surgery (e.g., fewer surgical excisions, less invasive procedures) and in anesthesia (anesthetics with a shorter half-life and minimal respiratory suppression) have made cancer surgery safer than ever for the elderly. Combined chemotherapy and radiation therapy in the management of cancers of the head and neck, the esophagus, the bladder, and the lung also appear to be well tolerated up to the age of 80 at least (Balducci and Beghé 2008). Balducci and Beghé (2008) states that the key to effective and safe treatment of elderly patients with cancer is informed decision making. Two components need to be looked at in the decision: the person and the malignancy. He asserts that cytotoxic chemotherapy is generally not indicated in a 90-year-old woman with stage 1 or 2 breast cancer because any benefit would be negligible and the risk of treatment would be considerable. He goes on to report that studies have shown that chemotherapy is of benefit to an 80-year-old woman whose chances of dying of breast cancer are only about 30% and if a 1% reduction in the cancer-related mortality is advantageous. However, in a 90-year-old woman, the risk of dying of breast cancer must be close to 70% to legitimize the use of chemotherapy. If the same patient has a chemotherapy-responsive disease, such as large cell non-Hodgkin's lymphoma that may shorten her life, then chemotherapy is definitely indicated. At times, it's best to go with the intuition of the patient. One 83-year-old man with an aggressive form of prostate cancer, in addition to mild cases of high blood pressure, Type 2 diabetes, depression, and angina---all being treated with medication---felt that hormone and radiation therapy was the way to go. Three months after finishing his therapy, blood tests suggested that the malignancy was eradicated (Brody 2009). More patients over 80 years undergo major cancer (and other) surgeries, when in the past the recommendation would have been to "let nature take its course" (Tampa Tribune 2009). However, doctors often under-treat the elderly for fear of the results of side effects. Other times they over-treat because of pressure from the family. Things that should influence treatment decisions are (Brody 2009) the patients':
Diseases of the Mind"Diseases of the mind" is, in a sense, a way of referring to the negative side mental health. When an elderly person seems to be "aging successfully" in mental and emotional areas, the social worker's job is largely one of encourager and cheerleader. When this aging is less successful, then the social worker's job is the same as when a physical illness is present: notice, aid the patient in getting professional help if it is needed, and help the client to engage in self-help strategies that might be useful.
Almost 20% of people ages 55 and older suffer mental disorders that are not part of normal aging. The most common disorders, in the order of predominance are: anxiety, severe cognitive impairment (e.g., dementia and Alzheimer's disease), and mood disorders (e.g., depression) (AAGP 2004). There is a difference between anxiety as a feeling or experience, and an anxiety disorder as a psychiatric diagnosis---an individual may feel anxious and not have an anxiety disorder. Primarily for this reason, anxiety is not addressed in this course. Aging and DepressionDepression in the aged is a significant problem. Changes in physical abilities, illnesses and diseases, the loss of loved ones, lack of a defining activity, and lack of work can all contribute to significant depressive feelings. Without a feeling of some purpose, many will not feel that getting out of bed in the morning is worth it, and depression can get worse as health declines.
Everyone, young or old, feels "down in the dumps" at times. But if they have little joy or pleasure from life, and the "down in the dumps" feeling lasts more than a week or two, they probably are depressed. Depression in the elderly needs to be diagnosed and treated. It could be a side-effect of a medication or a disease such as Parkinson's. But no matter the cause it can likely be treated. The risk of depression in the elderly increases just as other illnesses do. When the inability to function is more limited than before, they are especially at risk. Estimates of major depression in older people who still live in the community range from less than 1% to about 5%, but it rises to 13.5% in those who require home health care and to 11.5% in elderly hospital patients (Hybels and Blazer 2003). The percentages of people with clinically relevant depressive symptoms, along with age groups are displayed for 2004 in the following table:
Source: Federal Interagency Forum 2008, Chart 2008-19b Depression is one of the conditions most commonly associated with suicide in older adults (Conway and Brent 1995). It is widely under-recognized and undertreated. Studies show that up to 75% of older adults who committed suicide visited a physician within a month before death (Conwell 2001). The rate of suicide is highest among the elderly as compared to any other age group; highest of all is the suicide rate for those 85 years and older---twice the overall national rate (AAGP 2004). These statistics show the urgency of learning to recognize and treat depression among older adults. [QN.No.#21.Up to 75% of older adults who committed suicide visited a physician within a month before death? true/false?] Depressive symptoms can be different in older adults than younger, often being masked under the resemblance to changes that occur with age. For example, older adults often have a natural tendency for lower appetite and a change in sleep pattern. It is important to do a complete psychosocial assessment, which includes a history of depressive symptoms. Common symptoms of depression are (Gallo and Katz n.d., MDConsult 2008):
[QN.No.#22.Symptoms for Major Depression include:] The cause(s) of clinical depression are not known. No biologic event or gene has been associated with depression; however, if there is a family history of depression, there seems to be an increased risk. Cerebrovascular disease, which is more common among the elderly, appears to play a role in late-onset depression---this has led to the "vascular depression hypothesis" (Conway and Steffens 1999). Treatment for Depression  The doctor will perform a complete physical examination, obtain laboratory tests, and assess mental status (ability to think clearly, remember, and make plans). The purpose of this workup is to determine if a medical condition or medication may be causing or contributing to the depression. Treatments for geriatric depression are much like those for the rest of the population:
Psychotherapy for depression can include (Alexopoulos et al 2001):
Educating the person and their family about depression are also important interventions. Cognitive therapy is one of the more common therapies used to help with depression. If not contraindicated by a client's mental capacity, it can be effective in alleviating or minimizing the depressive symptoms. In cognitive restructuring the professional helps the client replace faulty thinking or misconceptions with beliefs and thoughts that are more aligned with reality, leading to enhanced functioning. The therapist helps people improve their self-dialogue, educating them that it is this inner dialogue that is affecting their depressed mood. Sometimes, in working with the elderly, much of their dialogue may be pessimistic and negative about the elderly person's life situation, and thoughts that their life has been a failure. The following steps are useful in cognitive restructuring (Cormier and Cormier 1979):
For other guidelines in helping the elderly and their families with depression, go to the following link: http://www.psychguides.com/Geriatric%20Depression%20LP%20Guide.pdf Memory ImpairmentOften memory suffers with age. For the majority, this impairment is mild and does not cause problems beyond being a nuisance. For others, the impairment is more severe and is troublesome both to family and to the patient. Sometimes the memory impairment creates an issue of safety when stoves are left on or the person wanders and gets lost. In even more severe cases the senior may not remember significant life experiences and/or lose the ability to identify loved ones, including children and spouse. Memory impairment that creates issues of safety often leads to the discussion of the need for alternative long term care. The following table provides an illustration of the frequency of memory problems among older Americans. Specifically it reports the percentage of people age 65 and older with moderate or severe memory impairment, by age group.
Source: Federal Interagency Forum 2006, 26 There are different studies that examine what causes memory impairment. According to Marsha K. Johnson (2003), Yale University, source monitoring has great impact in how someone remembers, and this function is processed by the frontal lobes. Being able to process information and then tie these experiences together so they make sense---such as the environment in which the memory occurred---is part of memory. For example, if somebody goes to the beach with friends, they will gather and process information: e.g., the friends there, the sights and sounds of the ocean and the wind, etc. Being able to tie all these details together helps people create accurate memories. Damage to the frontal lobes can cause a person to gather less specific information, resulting in a less accurate memory and even false memories. Johnson elaborates: "Neuro-imaging experiments along with the patient data suggest that the frontal lobes are important in monitoring the source of memory. So, we . . . know that older adults do less well under certain circumstances in source monitoring tasks than do healthy, young adults. They are poorer on source recognition than on old-new recognition. Investigators have suggested that this occurs because the frontal lobes are among the slower to mature regions, and they are also more likely to show increasing neuropathology with age" (Johnson 2003). Dementia, Alzheimer's DiseaseThere are many similarities between dementia and Alzheimer's disease; it is necessary to know what the differences are. Alzheimer's is one kind of dementia---the most common one. In addition to Alzheimer's, dementias related somewhat to age include (Health-cares.net 2005):
[QN.No.#23.Not everyone with Parkinson has dementia.true or False?] Alzheimer's is a progressive and fatal brain disease that gradually destroys a person's memory, ability to learn and make judgments, etc. The disease kills brain cells that eventually will kill a person if they do not die first of something else. The progress of the disease can take from 3-20 years (ALZ 2008). Although a person may have recently been diagnosed with the disease, the progress of the disease may actually be advanced. Early warning signs of the disease include (ALZ 1999):
[QN.No.#24.Early signs of Alzhemier's disease include:] The changes that occur as a result of Alzheimer's can affect both the diagnosed individual and loved ones. Reactions to these changes can include depression, anxiety, fear, embarrassment, shame, isolation, loneliness, and feeling of loss. In response to these reactions the Alzheimer's Association suggests the following ways a healthcare professional can help (ALZ 1999):
DrugsThis is the age of polymedicine which is the direct result of disease states, multiple healthcare providers, inappropriate and/or self prescribing, and numerous prescriptions (Solomon 2000). This has made administering medications for the elderly one of the most difficult areas in their medical care. Major contributing factors are:
[QN.No.#25.Administering medications for the elderly is difficult because of which factors?] Together, these factors add to the heightened frequency of drug interactions and adverse drug responses in these patients (Diasio 2007). Medications no longer include prescription drugs and aspirin over the counter (OTC), but a multiplicity of OTC and herbal remedies as well. There are a number of reasons for sometimes dramatic pharmacokinetic changes with age. The most basic are:
The pharmacodynamic changes with age are basically because of alterations in the responsiveness of the target organ. Even if the pharmacokinetics are unchanged, they necessitate using smaller drug doses in the elderly (Diasia 2007). Medication ManagementBecause of the difficulties mentioned above, individuals involved in medication management for the elderly, need to be aware of several things. You, as a social worker or therapist, may need to confront a physician regarding these things, as one therapist did---with negative results to herself. She was a licensed mental health therapist with an M.S. degree in Counseling and Human Resource Development. At one point she was given the assignment to go to a nursing home to do an annual evaluation for the payor of a patient's care. She was to interview the patient, study all of the patient's records at the necessary to accomplish this. [QN.No.#26.You, as a health care professional, will never need to confront a physician regarding medication management.True/False] On reviewing the records she noted the huge numbers of medications being given and that many were prescribed over the phone when nurses called with a new complaint of the patient. The physician had seldom seen the patient. The therapist called the doctor to ask about the medications, but he was curt and unwilling to give adequate answers. Being a thorough person, the therapist looked every drug up in the Physicians' Desk Reference (PDR) and found that the concurrent use of two of them required a blood test being taken every six months. No blood tests had ever been taken in the more than eighteen months the two medications were used. This was noted in her report, with quotations from the PDR to substantiate it. The therapist was remanded for practicing medicine without a license, and the center for which she worked changed the rules to only allow therapists whose degree was in psychology to perform these evaluations in the future. (But the patient's blood was checked!) With this story in mind, be aware---unhesitatingly---of the following information. First, there are several basic principles that pertain to drug use in the elderly (Diasio 2007):
[QN.No.#27.Which of the following is important for you about, in regards to what the client is taking?] Some steps that can be taken to help prevent drug interactions are (Diasio 2007):
[QN.No.#28.To help prevent drug interactions, as a health care worker, you need to:] It is very important that you know, or know enough to realize you should find the interactions and side effects of the medications your clients are taking, especially those most commonly prescribed to older adults. Make a chart of the interactions and side effects of these 20 medications most often prescribed to older adults (Solomon 2000): 
Only a relatively small group of drugs causes most of the well-known adverse drug effects---every drug has side effects and can potentially cause an adverse drug response. Even if a particular drug has not had an adverse response reported, the physician needs to be aware that it could still take place. Diasio (2007) lists the following information about clinical presentations associated with adverse drug responses.
Practitioners need to be aware of the drugs that are potentially contraindicated in elderly patients (Col et al 1990):
Some drugs and combinations of OTC, prescription, and herbal drugs should be avoided because of potential drug interactions, for example (Col et al 1990):
[QN.No.#29. The client should not use garlic if he/she is taking which medications?] For a more complete list, go to the University of Michigan Health System's Website at http://www.med.umich.edu/1libr/aha/umherb01.htm. Compliance Issues One definition of medication compliance is "the extent to which a person's behavior coincides with medical or health advice" (Coates n.d.). Patient compliance to a medication procedure has become more of a problem over time. The reasons are multiple, but perhaps fixed income leads the pack. However good the reason, noncompliance can lead to a number of problems (Coates n.d.):
[QN.No.#30.Medication noncompliance can lead to:] Herrick (2006) has an outstanding booklet with very specific ways and helps to reduce drug costs. He sums some of it up in the following chart: Checklist for Saving Money on Drugs
Opportunities for Saving Money on a Brand-Name Drug
Checklist for Saving Money on Drugs Opportunities for Saving Money on a Brand-Name Drug Opportunities for Saving Money by Drug Substitution
1 Consumers should exercise caution to ensure that any Internet-based drug supplier is reputable. Patients using multiple drug sources should inform all pharmacies of all medications taken in order to prevent adverse drug interactions. From Herrick 2006
Kane et al (2004) offers the following strategies to improve compliance in the geriatric population:
To give a little different point of view as to how you can help your clients to improve their medication compliance and thus reduce the risk of adverse reactions, Solomon (2000) suggests:
Alcohol and Substance Abuse Issues among ElderlyThe phrase substance abuse brings to mind out-and-out alcoholics, "shoot 'em up" druggers, and other extremes. Although it is estimated that up to 17% of Americans 65 years or older have problems with alcohol (Task Force n.d.), that does not mean they are all alcoholics. Alcohol used in combination with certain medications can cause harmful effects--- including impaired coordination and cognition (Breslow et al 2003)---and elders that use these combinations can be defined as substance misusers and are generally classified as substance abusers. That is possibly why the statistics of alcohol and drug abuse are so high. Besides potential interactions with medications, there are other reasons why seniors should not use alcohol, or use it very sparingly. Elderly men (and women of all ages) have a smaller volume of total body water than younger men, so they reach a higher blood alcohol concentration from the same amount of alcohol consumption (Kalant 1998). Body composition continues to change with age; therefore, the effects of alcohol may be greater for an 80-year-old than for a 70-year-old (Vestal et al 1977). This tends to result in more harm from the same amount of intake as compared to younger people. Other vulnerabilities of the elderly to the effects of alcohol may be raised by age-related changes in functional status, nutritional status, and psychological and cognitive status (Breslow et al 2003). With these concerns in mind, it is important to note that heavier use (which is not as heavy for the elderly) of alcoholic beverages has been linked with a number of detrimental health consequences, including cirrhosis of the liver, motor vehicle crashes and other unintentional injuries (NIAAA 2000), as well as with hemorrhagic and ischemic stroke (Reynolds et al 2003). Other reports indicate that the consumption of three to five drinks per day over years has been associated with an increase in the death rate (Yee and Williams 2002, 265). On the other hand, light or moderate consumption (one drink per day at most) has been linked with some health benefits, including reduced rates of coronary heart disease (Mukamal et al 2003)---this may be due to the antioxidants and resveratrol content of red wine which can be obtained through safer means (Mayo 2009a). Moving from alcohol misuse or abuse to drug abuse---again the biggest problem for seniors is drug misuse. A client who does not take medications as prescribed---forgetting to take them or taking extra because "if a little is good for me, a lot must be better"---is a drug misuser. That is why it is so important to oversee and regularly monitor their medication use. As with other populations, there are situations that tend to motivate some elderly persons to drink. Four factors that may cause the elderly to be susceptible to drinking alcohol or abusing some drugs are (Brody 1980):
Perhaps the greatest situational motivator of all is depression (Whelan 2003), which has been discussed earlier in this course. When an older person is amenable to treatment for substance use problems, they usually have better success in treatment than do younger people according to Frederic Blow, professor in the Department of Psychiatry at the University of Michigan and a Huss Research Chair on Older Adults and Alcohol/Drug Problems at Hazelden's Butler Center for Research (Hazelden 2006). If clients or their relatives need help and intervention for substance use, Hazelden has an outstanding pamphlet with information and suggestions, How to Talk to an Older Person Who Has a Problem with Alcohol or Medications, available at http://www.hazelden.org/web/public/document/ip_talkolderperson.pdf. Health and NutritionWhether you prefer Anthelme Brillat-Savarin's 1826 statement, "Tell me what you eat and I will tell you what you are," or the way the nutritionist Victor Lindlahr put it in 1923, "Ninety per cent of the diseases known to man are caused by cheap foodstuffs. You are what you eat," you recognize the same truth in both statements: the food that a person eats is foundational to the person's state of mind and health---that to be fit and healthy one needs to eat good food (Martin n.d.). Few people dispute that fact. Any disagreements would be in the areas of what fulfills the category of "good food." What is good for some is not necessarily good for all. And the elderly definitely do have some nutritional needs that are unique to them. Nutritional Needs of the Elderly
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
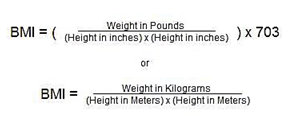
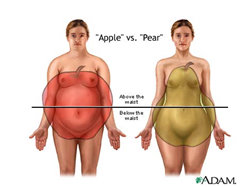
| Classification of Overweight and Obesity by BMI, Waist Circumference, and Associated Disease Risks | ||||
|---|---|---|---|---|
| Disease Risk* Relative to Normal Weight and Waist Circumference | ||||
| BMI (kg/m2) | Obesity Class | Men 102 cm (40 in) or less Women 88 cm (35 in) or less | Men > 102 cm (40 in)Women > 88 cm (35 in) | |
| Underweight | < 18.5 | - | - | |
| Normal | 18.5 - 24.9 | - | - | |
| Overweight | 25.0 - 29.9 | Increased | High | |
| Obesity | 30.0 - 34.9 | I | High | Very High |
| 35.0 - 39.9 | II | Very High | Very High | |
| Extreme Obesity | 40.0 + | III | Extremely High | Extremely High |
+ Increased waist circumference can also be a marker for increased risk even in persons of normal weight.
Overweight and Obesity
Unless an elderly person is obese, he/she probably does not need to lose weight according to one meta-analysis study (Asefeh et al 2001). The conclusion of the study said, "Evidence does not support mild-to-moderate overweight, defined by the new guidelines, as a risk factor for all-cause and cardiovascular mortality among elderly persons. We agree that marked overweight (obesity) might be a risk factor for this population. However, adverse effects of energy (calorie) restriction in elderly persons and the potential harms of diet-induced weight reduction, as well as the paucity of information about effectiveness of weight loss programs, would not support weight reduction interventions among mildly to moderately overweight elderly individuals."
Harlan M. Krumholz, the study's senior author, stated, "We found that in general, higher weight is associated with a smaller excess risk in older people compared with younger people" (Yale 2001).
Additionally, repeated dieting with weight loss followed by weight gain is bad for one's health. The Medical University of South Carolina discovered that "weight fluctuation is associated with a higher risk of all-cause and cardiovascular disease mortality in the U.S. population, even after adjustment for pre-existing disease, initial BMI and the exclusion of those in poor health or incapacitated. Thus, health care providers should promote a commitment to maintaining weight loss to avoid weight fluctuation and consider patients' weight histories when assessing their risk status" (Diaz et al 2005).
The U.S. Department of Health and Human Services and the U.S. Department of Agriculture (HHS & USDA 2005) make the following recommendation to " sustain weight loss in adulthood: Participate in at least 60 to 90 minutes of daily moderate-intensity physical activity while not exceeding caloric intake requirements. Some people may need to consult with a healthcare provider before participating in this level of activity."
Sometimes, however, there is unplanned weight loss.
Weight Loss and Cachexia
Many people who are not elderly may wish they had unintentional weight loss, because intentional doesn't seem to work very well. Unfortunately, unintentional weight loss, particularly cachexia (which includes wasting loss of fat and muscle), at any age is usually associated with illness and/or other problems. The cause of cachexia in the elderly is associated with increased morbidity and mortality. But it is hard to identify the cause, especially if the individual has multiple medical problems and is taking numerous medications, and especially if there is cognitive debilitation (Huffman 2002).
In addition to unintentional weight loss, cachexia is associated with one or more of the following symptoms and/or consequences ((Wikipedia 2009; Lewko et al 2003):
- Muscle atrophy (always occurs in cachexia), and wasting of fat
- Fatigue
- Weakness
- Significant loss of appetite
- Anemia
- Decreased cognition
- Edema
- Falls
- Hip fractures
- Immune dysfunction
- Infections
- Muscle loss
- Osteoporosis
- Pressure sores
There are numerous potential causes for cachexia. A mnemonic for common treatable causes of unintentional weight loss in the elderly is MEALS ON WHEELS (Huffman 2002):
| "Meals on Wheels": A Mnemonic for Common Treatable Causes of Unintentional Weight Loss in the Elderly | |
|---|---|
| M | Medication effects |
| E | Emotional problems, especially depression |
| A | Anorexia nervosa, alcoholism |
| L | Late-life paranoia |
| S | Swallowing disorders |
| O | Oral factors (e.g., poorly fitting dentures, caries) |
| N | No money |
| W | Wandering and other dementia-related behaviors |
| H | Hyperthyroidism, hypothyroidism, hyperparathyroidism, hypoadrenalism |
| E | Enteric problems |
| E | Eating problems (e.g., inability to feed self) |
| L | Low-salt, low-cholesterol diet |
| S | Stones (cholecystitis), social problems (e.g., isolation, inability to obtain preferred foods) |
Adapted with permission from Morley JE, Silver AJ. Nutritional Issues in Nursing Home Care.
Ann Intern Med 1995;123:850-9, with additional information from Reife CM.
Involuntary Weight Loss. Med Clin North Am 1995;79:299-313
Ann Intern Med 1995;123:850-9, with additional information from Reife CM.
Involuntary Weight Loss. Med Clin North Am 1995;79:299-313
In addition to the problems listed with the mnemonic, other studies have found that unintentional weight loss may be a preclinical indicator of Alzheimer's disease and that the weight loss often accelerates before diagnosis (Stewart et al 2005; Johnson et al 2006).
Protein-Energy Malnutrition
(Merck 2007)
Protein-energy malnutrition (PEM) refers to a form of malnutrition where there is inadequate protein intake, sometimes also called protein-calorie malnutrition. At times a person may ingest enough calories but not enough protein, which causes pure protein deficiency, but usually both deficiencies occur. Some individuals may get PEM not from inadequate ingestion but because they are unable to absorb protein (and probably other nutrients) or convert them into the energy needed to form healthy tissue or enable organs to function properly.
Primary PEM is the result of a diet lacking enough sources of protein and/or energy. Secondary PEM is the more common form that appears in the United States, and is usually a complication of AIDS, cancer, chronic kidney failure, inflammatory bowel disease, and other illnesses that hinder the body's ability to absorb or use nutrients or to compensate for nutrient losses.
In the U.S., PEM occurs most commonly in elderly people who live in nursing homes. It also occurs in 50% of surgical patients and 48% of all other hospital patients.
Secondary PEU is most commonly caused by:
- Disorders that affect GI function; these disorders can interfere with digestion (e.g., pancreatic insufficiency), absorption (e.g., enteritis, enteropathy), or lymphatic transport of nutrients (e.g., retroperitoneal fibrosis, Milroy's disease)
- Wasting disorders such as AIDS or cancer
- Conditions that increase metabolic demands, including infections, hyperthyroidism, pheochromocytoma, other endocrine disorders, burns, trauma, surgery, and other critical illnesses.
In a patient with a chronic illness or who has chronic semi-starvation, PEM can gradually evolve. In a patient with an acute illness it may appear abruptly.
Secondary PEM symptoms range from mild to severe; they can change the form or function of just about every organ in the body. The nature and severity of the symptoms are influenced by patient's prior nutritional status, the makeup of the underlying disease and how fast it is progressing.
Individuals who unintentionally lose 10-20% of their body weight, have a weakened grip, and are unable to perform high-energy tasks are said to have moderate secondary PEM. This also fits the description of cachexia.
A person with severe secondary PEM will have lost 20% or more of body weight, and are unable to eat normal-size meals. They also have low blood pressure and body temperature, and slow heart rates. They may also have:
- Baggy, wrinkled skin
- Constipation
- Dry, thin, brittle hair
- Lethargy
- Pressure sores and other skin lesions
Most people can unintentionally lose up to 10% of their body weight without side effects; the loss of more than 40% is almost always fatal. In these cases death usually results from heart failure, an electrolyte imbalance, or low body temperature. Patients with the poorest prognosis have particular symptoms, including:
- Semiconsciousness
- Persistent diarrhea
- Jaundice
- Low blood sodium levels
If you have clients that begin to have symptoms of malnourishment, notify their physicians as soon as possible. They are likely aware of the problem, but if not will design a treatment to give adequate nutrition, restore normal body composition, and cure the condition that caused the deficiency. For patient who can't or won't eat protein-rich foods, tube or intravenous feeding may be used to furnish needed nutrients (Gale Encyclopedia 2008).
Food Safety
In addition to adequate nutrient intake, food safety is also to be recognized. From January 24 through March 27, 2009---a period of sixty days, over 550 food products were recalled in the U.S. ("the most significant product actions"), some voluntary and some involuntary, many based on a recall of the manufacturer of an ingredient, such as the peanut factory recall during that time (FDA 2009).
With this quantity of recalls, it is impossible for the average American, let alone the elderly, to never risk eating contaminated food. Also, the elderly population is more at risk to food-borne illness, because (FDA 2001):
- The immune system no longer functions at optimal levels.
- The lining of the stomach often is somewhat inflamed, and there is a reduction in stomach acids.
- There is often a lack of good and/or sufficient nutrition.
While a wide variety of foods is best for optimal nutrition, the FDA warns that seniors should not eat (FDA 2001):
- Raw fin fish and shellfish, including oysters, clams, mussels, and scallops.
- Raw or unpasteurized milk or cheese.
- Soft cheeses such as feta, Brie, Camembert, blue-veined, and Mexican-style cheese. (Hard cheeses, processed cheeses, cream cheese, cottage cheese, or yogurt need not be avoided.)
- Raw or lightly cooked egg or egg products including salad dressings, cookie or cake batter, sauces, and beverages such as eggnog.
- Raw meat or poultry.
- Raw alfalfa sprouts which have only recently emerged as a recognized source of food-borne illness.
- Unpasteurized or untreated fruit or vegetable juice. When fruits and vegetables are made into fresh-squeezed juice, harmful bacteria that may be present can become part of the finished product. Most juice in the United States, 98%, is pasteurized or otherwise treated to kill harmful bacteria. To help consumers identify unpasteurized or untreated juices, the Food and Drug Administration is requiring a warning label on these products. The label says:
[QN.No.#31.The FDA warns that seniors should not eat (FDA 2001):]
WARNING:
This product has not been pasteurized and therefore may contain harmful bacteria that can cause serious illness in children, the elderly, and persons with weakened immune systems. - CLEAN: Wash hands and surfaces often. Bacteria can spread throughout the kitchen and get onto cutting boards, utensils, sponges and counter tops. Here's how to Fight BAC:
- Wash your hands with hot soapy water before handling food and after using the bathroom, changing diapers and handling pets.
- Wash your cutting boards, dishes, utensils and counter tops with hot soapy water after preparing each food item and before you go on to the next food.
- Use plastic or other non-porous cutting boards. These boards should be run through the dishwasher -- or washed in hot soapy water -- after use.
- Consider using paper towels to clean up kitchen surfaces. If you use cloth towels, wash them often in the hot cycle of your washing machine.
- SEPARATE: Don't cross contaminate Cross-contamination is the scientific word for how bacteria can be spread from one food product to another. This is especially true when handling raw meat, poultry and seafood, so keep these foods and their juices away from ready-to-eat foods. Here's how to Fight BAC:
- Separate raw meat, poultry and seafood from other foods in your grocery shopping cart and in your refrigerator.
- If possible, use a different cutting board for raw meat products.
- Always wash hands, cutting boards, dishes and utensils with hot soapy water after they come in contact with raw meat, poultry and seafood.
- Never place cooked food on a plate which previously held raw meat, poultry or seafood.
- COOK: Cook to proper temperatures Food safety experts agree that foods are properly cooked when they are heated for a long enough time and at a high enough temperature to kill the harmful bacteria that cause food-borne illness. The best way to Fight BAC is to:
- Use a clean thermometer, which measures the internal temperature of cooked foods, to make sure meat, poultry, casseroles and other foods are cooked all the way through.
- Cook roasts and steaks to at least 145°F. Whole poultry should be cooked to 180°F for doneness.
- Cook ground beef, where bacteria can spread during processing, to at least 160°F. Information from the Centers for Disease Control and Prevention (CDC) link eating undercooked, pink ground beef with a higher risk of illness. If a thermometer is not available, do not eat ground beef that is still pink inside.
- Cook eggs until the yolk and white are firm. Don't use recipes in which eggs remain raw or only partially cooked.
- Fish should be opaque and flake easily with a fork.
- When cooking in a microwave oven, make sure there are no cold spots in food where bacteria can survive. For best results, cover food, stir and rotate for even cooking. If there is no turntable, rotate the dish by hand once or twice during cooking.
- Bring sauces, soups and gravy to a boil when reheating. Heat other leftovers thoroughly to 165°F.
- CHILL: Refrigerate promptly
-
- Refrigerate or freeze perishables, prepared food and leftovers within two hours.
- Never defrost food at room temperature. Thaw food in the refrigerator, under cold running water or in the microwave. Marinate foods in the refrigerator.
- Divide large amounts of leftovers into small, shallow containers for quick cooling in the refrigerator.
- Don't pack the refrigerator. Cool air must circulate to keep food safe.
Refrigerate foods quickly because cold temperatures keep harmful bacteria from growing and multiplying. So, set your refrigerator no higher than 40°F and the freezer unit at 0°F. Check these temperatures occasionally with an appliance thermometer. Then, Fight BAC by following these steps:
-
[QN.No.#32.scientific word for how bacteria can be spread from one food product to another.]
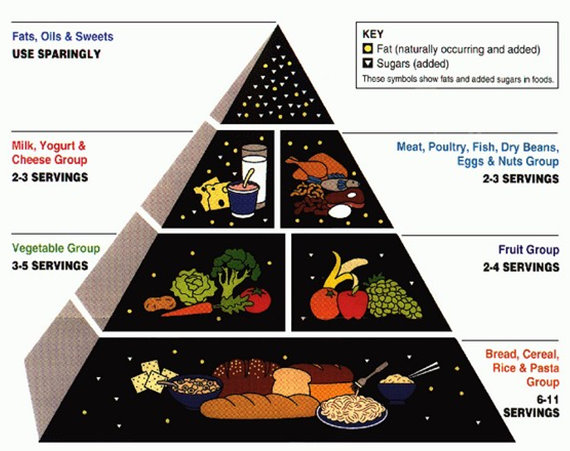
Finding an Eating Plan
In these days of the Internet, individuals can find an eating plan for any philosophy they choose. Many are healthy diets, many are not---and many of those are simply fads. The U.S. Department of Health and Human Services and the U.S. Department of Agriculture jointly recommend using either the USDA Food Guide or the DASH Eating Plan (HHS & USDA 2005).
The USDA food guide has been discussed earlier when their food pyramid was presented, so it will not be further considered here.
The DASH diet formed the basis for the USDA MyPyramid (DASH 2009), so it also many not be adapted for seniors, but guidelines given earlier should be used. The basic diet is:
| Type of food | Number of servings for 1600 - 3100 Calorie diets | Servings on a 2000 Calorie diet |
| Grains and grain products (include at least3 whole grain foods each day) | 6 - 12 | 7 - 8 |
| Fruits | 4 - 6 | 4 - 5 |
| Vegetables | 4 - 6 | 4 - 5 |
| Low fat or non-fat dairy foods | 2 - 4 | 2 - 3 |
| Lean meats, fish, poultry | 1.5 - 2.5 | 2 or less |
| Nuts, seeds, and legumes | 3 - 6 per week | 4 - 5 per week |
| Fats and sweets | 2 - 4 | limited |
Another excellent plan is presented by Dr. Eric R. Braverman in Younger You: Unlock the Hidden Power of Your Brain to Look and Feel 15 Years Younger (2007) and Younger You: Unlock the Hidden Power of Your Brain to Look and Feel 15 Years Younger (2009). Dr. Braveman focuses on nutrient-dense foods that together restore hormonal balance of the brain and improve health and aid in weight loss if that is needed.
Nutritional Supplements
There are those who strongly advocate taking nutritional supplements; there are those who advocate just as strongly against them, stating that people can get all the nutrients they need from food. You can find experiences of people on both sides, but many who take supplements have astounding stories, whereas those who do not take them also seldom have astounding stories. A 2007 survey (Williams) found that, of 1,202 adults under 60 years of age and 528 who were 60+, there were significantly more people who regularly took vitamin and mineral supplements than those who took them only occasionally or never took them. Those who took them regularly also (Williams 2007):
- Relied heavily on the medical profession for general health information
- Obtained supplements and diet information from diet books and periodicals
- Believed that taking vitamins and minerals prevented serious illness; reduced stress; prevented colds, skin problems, heart attacks, cancer, and other health problems
- Believed their overall well-being was improved through the use of supplements, but apparently did not believe that the use of supplements ensured good health.
- Did not seem to believe that the current food supply filled nutritional needs.
Whether or not one can get proper nutrition from foods alone takes one to the argument regarding organic vs. non-organic foods. One meta-analysis of studies on this topic says in the abstract (Heaton 2002):
"Any attempt to answer the question ‘is organic food better for you?’ requires an assessment of the safety, nutritional content and biological value aspects of food quality. Previous reviews have been unable to reach definitive conclusions after failing to ensure only valid comparisons are considered. When methodologically flawed studies are screened out and a complete assessment of nutritional quality is made, collectively, the available evidence supports the hypothesis that organically produced food is superior in terms of safety, nutritional content and nutritional value to that produced non-organically."
Rather than get in the fray, the best procedure for you is to help them get the best they can from food; if they want food supplements, help them find the best there---there are huge differences in quality and effectiveness between different supplements.
Exercise
In the last number of years, it has become well known that moderate exercise can significantly improve one's health and extend life. Physical inactivity is associated with increased incidence rates of obesity, diabetes, cardiovascular diseases, osteoporosis, and cancer; however, increased physical activity in middle age is eventually followed by a reduction in mortality to the same level as seen among men with constantly high physical activity. This reduction is comparable with that associated with smoking cessation (Byberg et al 2009).
For most elderly people, aerobic exercise (considered strenuous exercise) is either intimidating or out-and-out impossible.
Some of the results of a comparison of 22 studies on various populations with a variety of moderate exercises show that some of the exercises done, both type and quantity, would offer excellent results for seniors (Simon 2006):
| Type and Amount of Activities | Observed Benefit |
| Walking at least 1 hour/week | 73% lower risk for sudden cardiac death |
| Walking at least 1 hour/week | 51% lower risk for coronary artery disease |
| Walking or biking at least 1 hour/week | 29% lower mortality rate |
| Exercising at least 30 minutes on at least 6 days/month | 43% lower mortality rate |
If the client is able to progress to 30 minutes of moderate exercise a day, they may experience some or all of the following benefits (Mayo 2008):
- Lower blood pressure
- Improve cholesterol
- Prevent or manage type 2 diabetes
- Manage weight (coupled with a healthy diet)
- Prevent osteoporosis
- Prevent cancer
- Maintain mental well-being
- Increase energy and stamina---a lack of energy often results from inactivity, not age
One of the easiest exercises for the elderly is whole body vibration (WBV). Whole body vibration, which is exactly what you would deduce from its name, is performed by standing on a vibrating platform. The individual may just stand there (or sit, if needed) or he or she may do simple exercise on it. Motors underneath the platform transfer to the person on the machine. Machines can be adjusted to change the intensity, and often the direction, of the vibrations.

The frequency is one of the most important factors involved; every person has his own muscle frequency (Rittweger 2004). The direction differences focus the exercise on different areas of the body. This type of mechanical stimulation generates acceleration forces acting on the body. These forces cause the muscles to lengthen, transfers a signal through the central nervous system to all of the muscles involved. This uses many more muscle fibers than a conscious, voluntary movement does (Issurin and Tenenbaum 1999).
Medical research reports on vibration exercise---often performed for just 3-4 minutes a day several days a week---benefits show the following benefits for seniors:
- Significant improvement in walking speed, step length, maximum standing time on one leg (Iwamoto et al n.d.)
- Improve elements of fall risk and health-related quality of life (Bruyere et al 2005)
- Performance gains in chair rising, 18% (Runge et al 2000)
For a huge list of scientific studies, go to http://www.hmgco.com/studies.html. They show numerous studies on WBV that show positive results in the areas of (we've not checked all of the links recently, so they may not all be current):

- Fitness
- Performance
- Blood circulation
- Bone density
- Falls prevention
- Flexibility/Mobility/Balance
- Hormonal response
- Metabolism
- Neurological conditions
- Osteoporosis
- Pain management
- Multiple sclerosis
- Parkinson's disease
- Medical conditions and rehabilitation
An initial output of about $600 is required, although the machines can go for many thousands of dollars. There are cheaper ones, but they are so lightweight that they tip easily. The highest it is necessary to pay is $1300 for a vibrator that has three different settings for direction of vibration. They all have variable speeds for vibration.
Other exercises recommended for the elderly are strength (e.g., with dumbbells), stretching, yoga, and Tai Chi. Some recommend, "Just move!"
You can find a short regimen of armchair exercises for less mobile seniors at http://www.articledashboard.com/Article/Armchair- Exercises-for-the-Elderly/553828.
Aging and Sexuality
Sexual desire and activity extend well into later life for both men and women. However, it can be affected by aging. One study (Bretschneider and McCoy 1988) found that approximately 63% of men aged 80 to 102 are still sexually active.
Of participants in another study (Sill 2005) the majority of the women, and almost a majority of men did not report a low level of sexual desire until age 75 or older.
Factors other than age that reduced sexual desire were:
- Illnesses and medications. There is a high incidence of decreased sexual desire in those who take antidepressant drugs (Kuzmarov and Bain 2008).
- Negative attitudes towards sex
- Lack of education
- Presence of partner
Sill (2005) also reported that other studies found hormones reduced sexual desire and activity in the elderly.
Age and Sexual Response
In elderly men, increased physical stimulation is needed to achieve and maintain erections; orgasms are not as intense. In women, after menopause there are changes because of estrogen reduction or deficiency (Meston 1997).
The extent that aging affects sexual function is largely dependent on psychological, pharmacological, and illness-related causes.
Bretschneider and McCoy (1988) found that for both men and women ages 80--102, the most common activity was touching and caressing with no sexual intercourse. Next was masturbation, and then sexual intercourse. Only touching and caressing declined significantly from the 80s to the 90s for men, but not for women. With the exception of touching and caressing and past enjoyment of sexual intercourse, men had more activity and enjoyment. Being married, extramarital sex, and church attendance were significantly related with continuing to perform and enjoy some sexual behaviors. Current physical and social factors were of more importance than past and present frequency of sexual behavior except for sexual intercourse.
General effects of aging include (Laflin 2002, 281-2):
- Men:
- Circulating testosterone is decreased but rarely contributes to erectile disorders in healthy aging men.
- Penile erection takes more time, and the erection may not be as hard as before; direct, continuous penile stimulation is usually required. The advent of drugs has aided in this area.
- Testicles do not increase in size; they elevate later and to a lesser degree.
- Nipple erection becomes less discernible.
- Ejaculatory control increases.
- Sex flush is rare in the elderly.
- Sense of ejaculatory inevitability is diminished or absent.
- Ejaculation is less powerful and orgasm is often less intense, consisting of one or two expulsive contractions vs. four major contractions followed by minor contractions over several seconds of younger men.
- Ejaculate is expelled with less force and contains less seminal plasma. Men do not become sterile because of age.
- Loss of erection after ejaculation and testicular descent occur rapidly.
- Refractory period between ejaculations is longer, generally 12 to 48 hours.
- Climax still provides extreme sensate pleasure.
- Women:
- Vaginal lubrication takes longer.
- The expansion of the vaginal barrel is reduced in length and width.
- The lining of the vagina begins to thin and becomes easily irritated.
- The bladder and urethra may become irritated during intercourse.
- Vaginal secretion becomes less acidic, increasing the possibility of vaginal infection.
- The uterus does not elevate as high.
- The labia majora loses fullness, the clitoral size decreases, and the clitoral hood and fat pad over the mons veneris atrophy.
- Orgasmic phase is shorter.
- Resolution phase occurs more rapidly.
- Capability for multiple orgasm remains.
Sexuality, Estrogen Replacement and Other Hormone Therapy
In some cases, decreased sexual desire in women may have a hormonal element; post-menopause, hypopituitarism, adrenal inefficiency, or surgical menopause may play a role, but the major factors are likely to reside in psychological and situational conditions.
How the decline in levels of estrogen and progesterone and the role of testosterone relate to female sexual functioning as aging advances is not wholly clear. It is known that estrogen replacement therapy will restore vaginal epithelial function, increase vaginal flow, and increase the sense of well-being, but whether or not it improves sexual function is uncertain (Kuzmarov et al 2008).
Estrogen replacement therapy (ERT) has been reported to improve sexual desire in a significant percent of women, but there are many who experience no response. There is apparently a significant subgroup of women, particularly those whose problem has been a loss of libido, whose sexual issues initially respond to ERT, but who later regress to their original problems (Sarrel 2000).
ERT may have other benefits. Some studies suggest that hormone replacement therapy may have a selective beneficial effect on verbal memory in older non-demented women (Maki et al 2001).
There has been a general belief that since testosterone has libido-enhancing properties, it might intensify currently declining sexual interest among women---at least among women who have a low testosterone-producing capability due to physiological or pathological reasons (Kuzmarov and Bain 2008).
Erectile Dysfunction
(Merck n.d.a)
When the soft spongy tissue in the shaft of a male penis fills with blood, causing the penis to enlarge, stiffen and become erect, you have what is called penile erection. Erectile dysfunction has been a commonly used phrase ever since the first advertisements of Viagra.
There are several kinds of causes of erectile dysfunction:
Treatment of erectile dysfunction has had radical changes in the last number of years. The patient's goals and desires and the risks of various options guide the choice of treatment.
When the soft spongy tissue in the shaft of a male penis fills with blood, causing the penis to enlarge, stiffen and become erect, you have what is called penile erection. Erectile dysfunction has been a commonly used phrase ever since the first advertisements of Viagra.
There are several kinds of causes of erectile dysfunction:
- Vascular disorders, the most frequent cause in the elderly.
- Neurologic disorders---penile sensitivity may diminish with age and contribute to erectile dysfunction.
- Endocrine disorders, of which the most common in elderly men is the ADAM (Androgen Deficiency in the Aging Male) syndrome.
- Structural abnormalities
- Drugs
- Psychologic disorders. Among the elderly, most erectile dysfunction is organic rather than psychologic.
Treatment of erectile dysfunction has had radical changes in the last number of years. The patient's goals and desires and the risks of various options guide the choice of treatment.
- Drugs
- Sildenafil---a common trade name is Viagra. However, it can cause problems with cardiac function and vision, as well as headaches, flushing, and dyspepsia.
- Alprostadil---common adverse effects are a penile burning sensation and aching; less common in priaprism.
- Testosterone therapy may help if the problem is libido or the erectile dysfunction is due to hypogonadism.
- Other means
- Constriction rings may be useful for men who can obtain erections but can't sustain them.
- Vacuum tumescent devises that increase penile engorgement by creating a vacuum or negative pressure, drawing blood into the penis.
- Permanent penile prostheses or implants, used when other treatments don't seem to work.
- Penile revascularization surgery, so far not found to have a high success rate.
Sex in Nursing Homes
Everyone has heard of "strange bedfellows." Is "senior care and sex" one of them? Well, perhaps not. Aging does not stop one from being a sexual being---nor does living in a nursing home. Sexuality doesn't always mean intercourse; many residents are lonely or depressed and looking for ways to relieve them---simple touching may be enough.
Nursing homes are beginning to come to grips with the fact of senior sexuality. Following the guidelines of a study by Kansas State aging experts, they are looking at the following goals:

- Through education and open discussion, make staff comfortable with talking about seniors' sexuality (Hamilton 2008).
- Explain what sexuality means for older adults.
- Identify barriers to fulfilling the sexual needs.
- Find strategies to help residents.
- Learn how to discern appropriate from inappropriate sexual behaviors.
- Clear up staff misconceptions; add a dose of humor.
- Once staff appreciate the seniors' needs to be sexual and to be touched, look at several issues:
- Residents' right to privacy
- Finding ways to give residents this privacy
- When is sex for a person with dementia consensual and when is it rape?
- Making sure the sex is safe---educate the residents about sexually transmitted diseases.
- Be prepared to answer resident's requests for
- Lubrication products
- Pornography
- Double beds
- Access to drugs like Viagra
If social workers have a nursing home client with an unmet sexual need, they must find a way to address that need (KSU 2008, Edwards 2003). They also recommend some steps for preparing food safely at home.
Aging and Long-Term Care (10 Hours) > Chapter 2, Part B
Page Last Modified On:
Deprecated: Function strftime() is deprecated in /home/devxspeedy/public_html/lib/smarty-3.1.34/libs/plugins/modifier.date_format.php on line 81
February 18, 2015, 08:41 AM
Deprecated: Function strftime() is deprecated in /home/devxspeedy/public_html/lib/smarty-3.1.34/libs/plugins/modifier.date_format.php on line 81
February 18, 2015, 08:41 AM