|
Aging and Long-Term Care (10 Hours) > Chapter 5
|
|
Chapter 5: Long-Term CareAs a result of diminished physical and mental capacities, long-term care becomes a necessity for many older people. This care can be provided in different settings and from different sources including the elderly moving in with family members or vice-versa, paid home healthcare nurses and skilled nursing facilities (nursing homes). The decisions regarding long-term care are difficult. It is a sign to the older person that they are no longer fully independent or self-sufficient. There are also emotional issues regarding whether family members or hired professional personnel will provide care, and what level of care is necessary. The decision to place the elderly person in a nursing home can be devastating. Family members often feel guilt, while the elderly person may feel unloved and rejected. Symptoms of depression, anger, resentment, and denial may be present. [QN.No.#46.Alternatives for long-term care include:] [QN.No.#47.Because of the clear need, long-term care decisions are easy to make.True/False] HomecareAs parents age and need assistance, adult children often consider taking elderly parent(s) into their own home. However, not everyone is a caretaker. Some can care-take children, but not people with special needs or illnesses, at any age. Others have no problem caring for an older person with whom they feel a soul connection (Crystalinks n.d.). Should family members decide to either move in with the elderly person, or have the elderly person move in with the family, there will be some significant home-life adjustments. As a result of frustration from losing their independence, the elderly person may become demanding and critical of the caregiver. Sometimes they can become abusive, even physically. The family now has another person to care for who is sometimes even more demanding than children. The elderly may depend primarily, or even exclusively, on the family for social interaction and may need help with various personal needs and hygiene. Besides feeling frustrated, this can also be embarrassing to the elderly person. In these situations, helping family members create and practice healthy styles of communication can go a long way in reducing frustrations. It is also important to link caregivers and the elderly to resources. There are senior centers where the elderly person can go during the day to enjoy interaction and age appropriate activities. There are also community caregiver support groups that can provide ideas and the emotional boost that is needed from time to time. One source of good information may be found at http://www.ndsu.edu/ndsu/aging/caregiver/pdf/family/module.pdf. Homecare ServicesThere are times when an elderly person is able to do most things for themselves and wish to remain independent. For this situation there are a number of options for someone to come to the home to provide specified types of help. If the older person can afford it, this can be a perfect solution. There are a number of options for pay, although many of them may be reduced in times like the current national financial crisis. Types of payers of home-care services include (Moffa-Trotter and Anemaet 2002, 371):
The following table shows examples of home care provided under several federal programs (Kane et al 2004, 418): 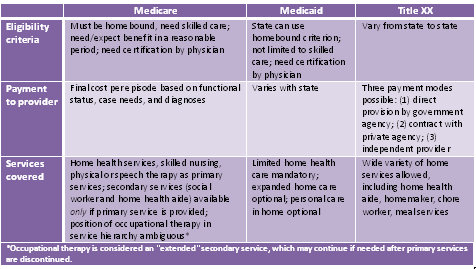 Home-Health AgenciesHome-health agencies are organizations that provide health care in the home. Medicare will certify a home-health agency if it offers skilled nursing services and at least one additional therapeutic service:
Homemaker and Homecare-Aide AgenciesMany of the homemaker and homecare-aide agencies are licensed; those are usually the ones that will also offer the best financing options. Many of them are under the auspices of a county. The following services are offered in various combinations, depending on the agency, to the qualified patient: 
Often the adult and aging sections of state departments of social services will have volunteers who will come in and act as a companion for a few hours a week, usually to give respite to a caretaking spouse. Independent ProvidersIndependent providers are private groups or individuals who offer many of the same services as those offered above. They usually require private pay. HospiceHospice is special care, either in the home or in a hospice facility, designed to comfort and support patients with limited life expectancy and their families. Patients are referred to hospice when life expectancy is about six months or less; to continue longer than six months, physician certification is required. [QN.No.#48.A Special care facility designed to comfort and support patients with limited life expectancy and their families:] Hospice care does not prolong life or hasten death. Its goal is to improve the quality of the patient's last weeks, days, or hours by offering comfort and dignity. They address all symptoms of disease with emphasis on controlling pain and discomfort (Hospice Foundation 2009). They can offer (AoA 2004):
Consider calling hospice when:
Wellness of Caregivers(NFCSP 2003)
Awareness of the difficulties of caregivers of elderly and ill people has come to light in recent years. Caregivers have identified some of the lessons they have learned:
[QN.No.#49.Which of the following is NOT good advice for a caregiver?] Factors that contribute to the physical and emotional stress that family caregivers experience include:
[QN.No.#50.Factors that contribute to the physical and emotional stress that family caregivers experience include:] Ways in which family caregivers can ease some of their caregiving burden and engage in more health-promoting and disease-prevention activities might include:
An excellent link for caregivers is: http://www.caregiver.com/. |
|
|
Aging and Long-Term Care (10 Hours) > Chapter 5
Page Last Modified On:
Deprecated: Function strftime() is deprecated in /home/devxspeedy/public_html/lib/smarty-3.1.34/libs/plugins/modifier.date_format.php on line 81 February 18, 2015, 09:41 AM |
|
