Chapter 2: Overview
A. About HIV & AIDS
1. What Are HIV and AIDS?
What Is HIV?
HIV (human immunodeficiency virus) is a virus that attacks cells that help the body fight infection, making a person more vulnerable to other infections and diseases. It is spread by contact with certain bodily fluids of a person with HIV, most commonly during unprotected sex (sex without a condom or HIV medicine to prevent or treat HIV), or through sharing injection drug equipment.
If left untreated, HIV can lead to the disease AIDS (acquired immunodeficiency syndrome).
The human body can't get rid of HIV and no effective HIV cure exists. So, once you have HIV, you have it for life.
However, by taking HIV medicine (called antiretroviral therapy or ART), people with HIV can live long and healthy lives and prevent transmitting HIV to their sexual partners. In addition, there are effective methods to prevent getting HIV through sex or drug use, including pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
First identified in 1981, HIV is the cause of one of humanity's deadliest and most persistent epidemics.
What Is AIDS? AIDS is the late stage of HIV infection that occurs when the body's immune system is badly damaged because of the virus. In the U.S., most people with HIV do not develop AIDS because taking HIV medicine every day as prescribed stops the progression of the disease. A person with HIV is considered to have progressed to AIDS when:
- the number of their CD4 cells falls below 200 cells per cubic millimeter of blood (200 cells/mm3). (In someone with a healthy immune system, CD4 counts are between 500 and 1,600 cells/mm3.) OR
- they develop one or more opportunistic infections regardless of their CD4 count.
Without HIV medicine, people with AIDS typically survive about 3 years. Once someone has a dangerous opportunistic illness, life expectancy without treatment falls to about 1 year. HIV medicine can still help people at this stage of HIV infection, and it can even be lifesaving. But people who start ART soon after they get HIV experience more benefits—that's why HIV testing is so important.
How Do I Know If I Have HIV? The only way to know for sure if you have HIV is to get tested. Testing is relatively simple. You can ask your health care provider for an HIV test. Many medical clinics, substance abuse programs, community health centers, and hospitals offer them too. You can also buy a home testing kit at a pharmacy or online. Content Source: HIV.gov Date last updated: June 17, 2019 https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/what-are-hiv-and-aids
2. How Is HIV Transmitted?
How Do You Get or Transmit HIV?
You can only get HIV by coming into direct contact with certain body fluids from a person with HIV who has a detectable viral load. These fluids are:
- Blood
- Semen (cum) and pre-seminal fluid
- Rectal fluids
- Vaginal fluids
- Breast milk
For transmission to occur, the HIV in these fluids must get into the bloodstream of an HIV-negative person through a mucous membrane (found in the rectum, vagina, mouth, or tip of the penis); open cuts or sores; or by direct injection. People with HIV who take HIV medicine daily as prescribed and get and keep an undetectable viral load have effectively no risk of sexually transmitting HIV to their HIV-negative partners. How Is HIV Spread from Person to Person? HIV can only be spread through specific activities. In the United States, the most common ways are:
- Having vaginal or anal sex with someone who has HIV without using a condom or taking medicines to prevent or treat HIV. Anal sex is riskier than vaginal sex.
- Sharing injection drug equipment (“works”), such as needles, with someone who has HIV.
Less common ways are:
- From mother to child during pregnancy, birth, or breastfeeding. However, the use of HIV medicines and other strategies have helped lower the risk of mother-to-child transmission of HIV to 1% or less in the United States.
- Getting stuck with an HIV-contaminated needle or other sharp object. This is a risk mainly for health care workers. The risk is very low.
HIV is spread only in extremely rare cases by:
- Having oral sex. But in general, the chance that an HIV-negative person will get HIV from oral sex with an HIV-positive partner is extremely low.
- Receiving blood transfusions, blood products, or organ/tissue transplants that are contaminated with HIV. The risk is extremely small these days because of rigorous testing of the U.S. blood supply and donated organs and tissues.
- Being bitten by a person with HIV. Each of the very small number of documented cases has involved severe trauma with extensive tissue damage and the presence of blood. There is no risk of transmission if the skin is not broken.
- Contact between broken skin, wounds, or mucous membranes and HIV-infected blood or blood-contaminated body fluids.
- Deep, open-mouth kissing if both partners have sores or bleeding gums and blood from the HIV-positive partner gets into the bloodstream of the HIV-negative partner. HIV is not spread through saliva.
- Eating food that has been pre-chewed by a person with HIV. The contamination occurs when infected blood from a caregiver's mouth mixes with food while chewing. The only known cases are among infants.
Does HIV Viral Load Affect Getting or Transmitting HIV?
Yes. Viral load is the amount of HIV in the blood of someone who has HIV. Taking HIV medicine (called antiretroviral therapy or ART) daily as prescribed can make the viral load very low—so low that a test can't detect it (this is called an undetectable viral load).
People with HIV who take HIV medicine daily as prescribed and get and keep an undetectable viral load have effectively no risk of transmitting HIV to an HIV-negative partner through sex.
HIV medicine is a powerful tool for preventing sexual transmission of HIV. But it works only as long as the HIV-positive partner gets and keeps an undetectable viral load. Not everyone taking HIV medicine has an undetectable viral load. To stay undetectable, people with HIV must take HIV medicine every day as prescribed and visit their healthcare provider regularly to get a viral load test.
Ways HIV Cannot Be Spread HIV is not spread by:
- Air or water
- Mosquitoes, ticks or other insects
- Saliva, tears, or sweat that is not mixed with the blood of a person with HIV
- Shaking hands; hugging; sharing toilets; sharing dishes, silverware, or drinking glasses; or engaging in closed-mouth or “social” kissing with a person with HIV
- Drinking fountains
- Other sexual activities that don't involve the exchange of body fluids (for example, touching).
HIV can't be passed through healthy, unbroken skin.
How Do You Get AIDS? You can't “catch” AIDS. AIDS is the most advanced stage of HIV infection. If you have HIV and you are not on HIV treatment, eventually your body's immune system will weaken and you will progress to AIDS. People with AIDS have such badly damaged immune systems that they get a number of severe illnesses, called opportunistic infections. People who are HIV-negative can prevent getting HIV by using PrEP (pre-exposure prophylaxis). Post-exposure prophylaxis (PEP) is a way to prevent HIV infection after a recent possible exposure to the virus. There are other ways to prevent getting or transmitting HIV through injection drug use and sexual activity. Content Source: HIV.gov Date last updated: June 24, 2019 https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/how-is-hiv-transmitted
3. Who Is at Risk for HIV?
HIV can affect anyone regardless of sexual orientation, race, ethnicity, gender or age. However, certain groups are at higher risk for HIV and merit special consideration because of particular risk factors. Is the Risk of HIV Different for Different People?
Some groups of people in the United States are more likely to get HIV than others because of many factors, including the status of their sex partners, their risk behaviors, and where they live.
When you live in a community where many people have HIV infection, the chances of having sex or sharing needles or other injection equipment with someone who has HIV are higher. You can use CDC's HIV, STD, hepatitis, and tuberculosis Atlas Plus to see the percentage of people with HIV (“prevalence”) in different US communities. Within any community, the prevalence of HIV can vary among different populations.
Gay and bisexual men have the largest number of new diagnoses in the United States. Blacks/African Americans and Hispanics/Latinos are disproportionately affected by HIV compared to other racial and ethnic groups. Also, transgender women who have sex with men are among the groups at highest risk for HIV infection, and injection drug users remain at significant risk for getting HIV.
Risky behaviors, like having anal or vaginal sex without using a condom or taking medicines to prevent or treat HIV, and sharing needles or syringes play a big role in HIV transmission. Anal sex is the highest-risk sexual behavior. If you don't have HIV, being a receptive partner (or bottom) for anal sex is the highest-risk sexual activity for getting HIV. If you do have HIV, being the insertive partner (or top) for anal sex is the highest-risk sexual activity for transmitting HIV.
But there are more tools available today to prevent HIV than ever before. Choosing less risky sexual behaviors, taking medicines to prevent and treat HIV, and using condoms with lubricants are all highly effective ways to reduce the risk of getting or transmitting HIV. Learn more about these and other strategies to prevent HIV.
Learn More About Groups at Risk for HIV For more information about the risk for different groups of people, see U.S. Statistics, Impact on Racial and Ethnic Minorities, and CDC's HIV by Geographical Distribution. For more information about groups at risk for HIV, visit CDC's Groups at Risk page. Content Source: HIV.gov Date last updated: May 15, 2017 https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/who-is-at-risk-for-hiv
1. Symptoms of HIV
How Can You Tell If You Have HIV?
The only way to know for sure if you have HIV is to get tested. You can't rely on symptoms to tell whether you have HIV. Knowing your HIV status gives you powerful information so you can take steps to keep yourself and your partner(s) healthy:
- If you test positive, you can take medicine to treat HIV. People with HIV who take HIV medicine daily as prescribed can live a long and healthy life and prevent transmission to others. Without HIV medicine (called antiretroviral therapy or ART), the virus replicates in the body and damages the immune system. This is why people need to start treatment as soon as possible after testing positive.
- If you test negative, there are several ways to prevent getting HIV.
- If you are pregnant, you should be tested for HIV so that you can begin treatment if you're HIV-positive. If an HIV-positive woman is treated for HIV early in her pregnancy, the risk of transmitting HIV to her baby can be very low.
Use the HIV Services Locator to find an HIV testing site near you. There are several symptoms of HIV. Not everyone will have the same symptoms. It depends on the person and what stage of the disease they are in. Below are the three stages of HIV and some of the symptoms people may experience. Stage 1: Acute HIV Infection Within 2 to 4 weeks after infection with HIV, about two-thirds of people will have a flu-like illness. This is the body's natural response to HIV infection. Flu-like symptoms can include:
- Fever
- Chills
- Rash
- Night sweats
- Muscle aches
- Sore throat
- Fatigue
- Swollen lymph nodes
- Mouth ulcers
These symptoms can last anywhere from a few days to several weeks. But some people do not have any symptoms at all during this early stage of HIV. Don't assume you have HIV just because you have any of these symptoms—they can be similar to those caused by other illnesses. But if you think you may have been exposed to HIV, get an HIV test.
- Request an HIV test for recent infection—Most HIV tests detect antibodies (proteins your body makes as a reaction to HIV), not HIV itself. But it can take a few weeks after you're infected for your body to produce them. There are other types of tests that can detect HIV infection sooner. Tell your doctor or clinic if you think you were recently exposed to HIV, and ask if their tests can detect early infection.
- Know your status—After you get tested, be sure to learn your test results. If you're HIV-positive, see a doctor as soon as possible so you can start treatment with HIV medicine. And be aware: when you are in the early stage of infection, you are at very high risk of transmitting HIV to others. It is important to take steps to reduce your risk of transmission. If you are HIV-negative, there are prevention options like pre-exposure prophylaxis (PrEP) that can help you stay negative.
Stage 2: Clinical Latency
In this stage, the virus still multiplies, but at very low levels. People in this stage may not feel sick or have any symptoms. This stage is also called chronic HIV infection.
Without HIV treatment, people can stay in this stage for 10 or 15 years, but some move through this stage faster.
If you take HIV treatment every day, exactly as prescribed and get and keep an undetectable viral load, you can protect your health and prevent transmission to others. But if your viral load is detectable, you can transmit HIV during this stage, even when you have no symptoms. It's important to see your health care provider regularly to get your level checked.
Stage 3: AIDS If you have HIV and you are not on HIV treatment, eventually the virus will weaken your body's immune system and you will progress to AIDS (acquired immunodeficiency syndrome). This is the late stage of HIV infection. Symptoms of AIDS can include:
- Rapid weight loss
- Recurring fever or profuse night sweats
- Extreme and unexplained tiredness
- Prolonged swelling of the lymph glands in the armpits, groin, or neck
- Diarrhea that lasts for more than a week
- Sores of the mouth, anus, or genitals
- Pneumonia
- Red, brown, pink, or purplish blotches on or under the skin or inside the mouth, nose, or eyelids
- Memory loss, depression, and other neurologic disorders
Each of these symptoms can also be related to other illnesses. The only way to know for sure if you have HIV is to get tested. Many of the severe symptoms and illnesses of HIV disease come from the opportunistic infections that occur because your body's immune system has been damaged. See your health care provider if you are experiencing any of these symptoms. Content Source: HIV.gov Date last updated: June 21, 2019 https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/symptoms-of-hiv
B. Data & Trends
1. U.S. Statistics
Fast Facts
Approximately 1.1 million people in the U.S. are living with HIV today. About 15 percent of them (1 in 7) are unaware they are infected. An estimated 38,700 Americans became newly infected with HIV in 2016. Gay, bisexual, and other men who have sex with men bear the greatest burden by risk group, representing an estimated 26,000 of new HIV infections per year.
- In 2017, 38,739 people received an HIV diagnosis in the U.S. and 6 dependent areas
- The annual number of new HIV diagnoses in the U.S. remained stable from 2012 to 2016.
- HIV diagnoses are not evenly distributed across states and regions. Of the 38,739 new HIV diagnoses in the U.S in 2017, 19,968 (52%) were in the South.
New HIV infections (“HIV incidence”) refers to the estimated number of people who are newly infected with HIV during a year, which is different from the number of people diagnosed with HIV during a year. (Some people may have HIV but not know it.)
According to the latest estimates from the Centers for Disease Control and Prevention (CDC):
Approximately 38,700 people became newly infected with HIV in the United States in 2016. After about 5 years of substantial declines, the number of annual HIV infections began to level off in 2013, to about 39,000 infections per year.
CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like blacks/African Americans and Hispanics/Latinos.
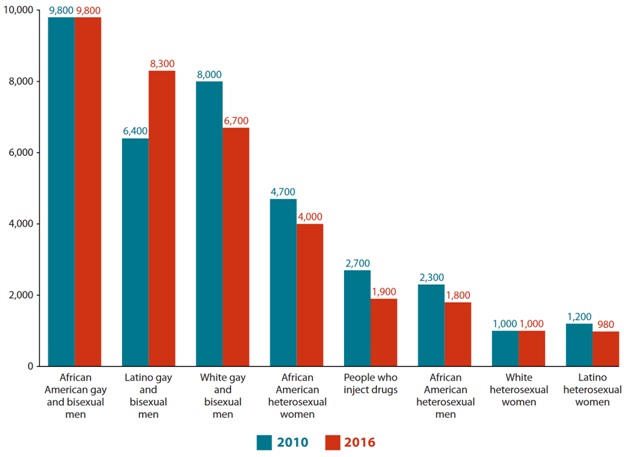
By age group, between 2010-2016, the annual number of HIV infections decreased among persons aged 13–24 and 45–54 but increased among persons aged 25–34. The number of infections remained stable among persons aged 33-44 and greater than or equal to 55 years.
By race/ethnicity, between 2010-2016, the annual number of HIV infections decreased among blacks/African Americans, whites, and persons of multiple races and remained stable for Asians and Hispanics/Latinos.
By sex, between 2010-2016, the annual number of new HIV infections decreased among females but remained stable among males.
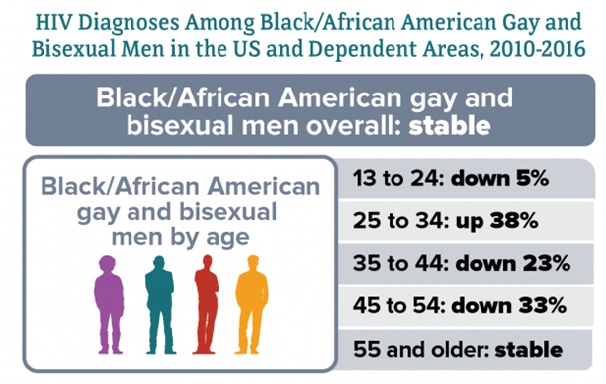
By HIV transmission category, between 2010-2016, the annual number of HIV infections decreased among male and female adults and adolescents with infection attributed to injection drug use, and among females with infection attributed to heterosexual contact. The annual number of infections remained stable overall among males with infection attributed to male-to-male sexual contact, among males with infection attributed to male-to-male sexual contact and injection drug use, and among males and females with infection attributed to injection drug use. However, there were differences by race/ethnicity and transmission group.
New HIV Infections by Race and Transmission Group, U.S. 2010 vs. 2016:
Source: CDC, HIV Incidence: Estimated Annual Infections in the U.S., 2010-2016, Feb. 2019.
HIV Diagnoses
HIV diagnoses refers to the number of people who have received an HIV diagnosis during a year, regardless of when they were infected. (Some people can live with HIV for years before they are diagnosed; others are diagnosed soon after infection.) According to the Centers for Disease Control and Prevention (CDC): In 2017, 38,739 people received an HIV diagnosis in the U.S. The annual number of new HIV diagnoses remained stable between 2012 and 2016 in the U.S. and dependent areas. However, annual new diagnoses have increased among some groups. HIV Diagnoses in the U.S. and Dependent Areas, 2012–2016
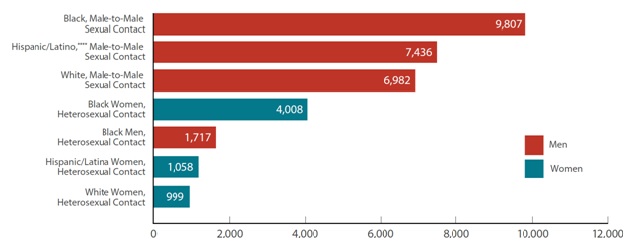
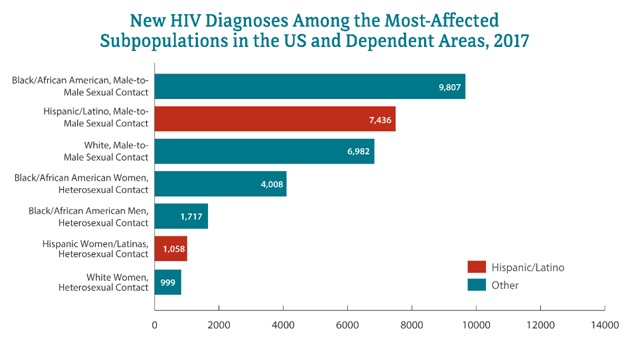
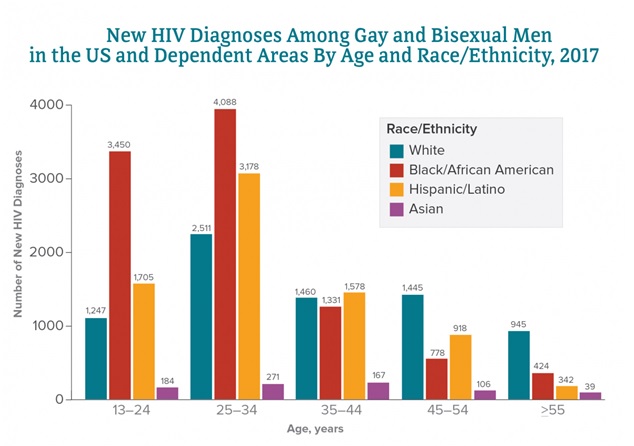
Source: CDC, HIV in the United States and Dependent Areas, Jan. 2019. Gay and bisexual men are the population most affected by HIV. In 2017:
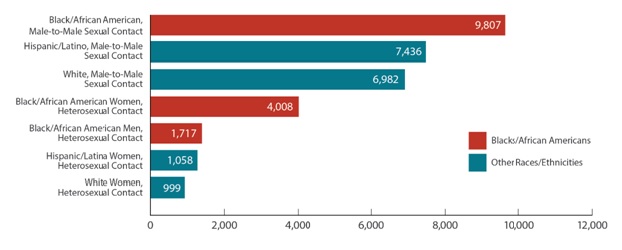
- Gay and bisexual men accounted for 66% (25,748) of all HIV diagnoses and 82% of HIV diagnoses among males.
- Black/African American gay and bisexual men accounted for the largest number of HIV diagnoses (9,807), followed by Hispanic/Latinos (7,436) and whites (6,982).
Among all gay and bisexual men, HIV diagnoses remained stable from 2012 to 2016, but trends varied by race/ethnicity:
- HIV diagnoses among white gay and bisexual men decreased 14%.
- HIV diagnoses among African American gay and bisexual men remained stable.
- HIV diagnoses among Hispanics/Latino gay and bisexual men increased 12%.
Heterosexuals and people who inject drugs also continue to be affected by HIV. In 2017:
- Heterosexuals accounted for 24% of HIV diagnoses.
- Heterosexual men accounted for 7% (2,829) of HIV diagnoses.
- Heterosexual women accounted for 16% (6,341) of HIV diagnoses.
- People who inject drugs accounted for 6% of HIV diagnoses.
From 2012 to 2016:
- HIV diagnoses among heterosexual women decreased 8%.
- HIV diagnoses among heterosexual men decreased 9%.
- HIV diagnoses among people who inject drugs decreased 17%
By race/ethnicity, African Americans and Hispanics/Latinos are disproportionately affected by HIV. In 2017:
- African Americans accounted for 43% (16,694) of HIV diagnoses and 13% of the population.
- Hispanics/Latinos accounted for 26% (9,908) of HIV diagnoses and 18% of the population.
From 2012 to 2016:
- HIV diagnoses among African Americans decreased 5%.
- HIV diagnoses among Hispanics/Latinos remained stable.
- HIV diagnoses among whites decreased 8%.
New HIV Diagnoses in the U.S. and Dependent Areas for the Most-Affected Subpopulations, 2017:
Source: CDC, HIV in the United States and Dependent Areas, Jan. 2019.
In the U.S., HIV diagnoses are not evenly distributed across states and regions.g In 2017, the South accounted for more than half (52%) of the new HIV diagnoses in the U.S., followed by the West (19%), the Northeast (16%), and the Midwest (13%). U.S. dependent areas made up 1% of new HIV diagnoses. Most infections are now highly concentrated in certain geographic hotspots. More than 50 percent of new HIV diagnoses in 2016 and 2017 occurred in 48 counties, Washington, D.C., and San Juan, Puerto Rico.
Living with HIV
In all 50 states and the District of Columbia:
- An estimated 1,122,900 adults and adolescents were living with HIV in the U.S. at the end of 2015.
- Of those, about 14% (or 1 in 7) had not received a diagnosis, so were unaware of their infection.
- Young people were the most likely to be unaware of their infection. In 2015, among people aged 13-24 who were living with HIV, an estimated 51% didn't know.
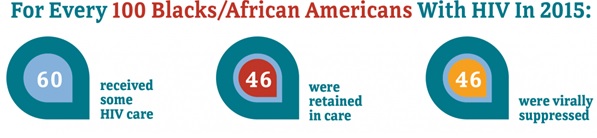
- In 2015, among all adults and adolescents living with HIV (diagnosed and undiagnosed),
- 63% received some HIV medical care,
- 49% were retained in continuous HIV care, and
- 51% had achieved viral suppression (having a very low level of the virus). A suppressed viral load protects the health of a person living with HIV, preventing disease progression. There is also a major prevention benefit. A person living with HIV who takes HIV medicine as daily prescribed and gets and stays virally suppressed can stay healthy and has effectively no risk of sexually transmitting HIV to HIV-negative partners.
AIDS Diagnoses and Deaths In 2017, 17,803 people in the U.S. and 6 dependent areas received a stage 3 (AIDS) diagnosis. In 2016, there were 15,807 deaths among people with diagnosed HIV in the United States. Nearly half (47%) of these deaths were in the South; 3,630 (23%) were in the Northeast; 2,604 (16%) were in the West; 1,720 (11%) were in the Midwest; and 379 (2%) were in the U.S. dependent areas. These deaths may be due to any cause. The ‘Ending the HIV Epidemic' Initiative Ending the HIV Epidemic: A Plan for America, announced by the President in his State of the Union address on February 5, 2019, is a bold approach to eliminate new HIV infections in our nation. It is built upon the following key strategies:
- Diagnosing all individuals with HIV as early as possible after infection.
- Treating HIV rapidly and effectively after diagnosis to achieve sustained viral suppression.
- Protecting individuals at risk for HIV using proven prevention approaches.
- Responding rapidly to detect and respond to growing HIV clusters and prevent new infections.
The proposed initiative is designed to rapidly increase use of these strategies in the 48 counties with the highest HIV burden, as well as in Washington, D.C.; San Juan, Puerto Rico; and seven states with a disproportionate rural HIV burden. The goal is to reduce new HIV infections by 90 percent over 10 years.
Notes
- Referred to as African American in this fact sheet.
- Hispanics/Latinos can be of any race.
- Unless otherwise noted, the term United States (U.S.) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the U.S. Virgin Islands.
- These numbers include only diagnoses attributed to male-to-male sexual contact, not those attributed to injection drug use and male-to-male sexual contact.
- This does not include gay and bisexual men who reported injection drug use. CDC's HIV surveillance fact sheet provides more information about how CDC classifies the transmission category for HIV cases.
- This does not include heterosexuals who reported injection drug use.
- This page uses the regions defined by the U.S. Census
Bureau and used in CDC's National HIV Surveillance System: Northeast: CT, ME, MA, NH, NJ, NY, PA, RI, VT Midwest: IL, IN, IA, KS, MI, MN, MO, NE, ND, OH, SD, WI South: AL, AR, DE, DC, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV West: AK, AZ, CA, CO, HI, ID, MT, NV, NM, OR, UT, WA, WY. Bibliography CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2016. HIV Surveillance Supplemental Report 2018;23(4). CDC. Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report 2019;24(No. 1) CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. CDC. Deaths: Final Data for 2014. National Vital Statistics Reports 2016;65(4). Content Source: Centers for Disease Control and Prevention Date last updated: March 13, 2019 https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
2. Impact on Racial and Ethnic Minorities
What Is the Impact of HIV on Racial and Ethnic Minorities in the U.S.?
In the United States, HIV is spread mainly through anal or vaginal sex or by sharing drug-use equipment with an infected person. Although these risk factors are the same for everyone, some racial/ethnic groups are more affected than others, given their percentage of the population. This is because some population groups have higher rates of HIV in their communities, thus raising the risk of new infections with each sexual or drug use encounter.
Additionally, a range of social, economic, and demographic factors—such as stigma, discrimination, income, education, and geographic region—affect their risk for HIV. To learn about the HIV prevention challenges for various racial and ethnic minorities in the United States, see the following CDC fact sheets:
HIV and African Americans
Blacks/African Americansa account for a higher proportion of new HIV diagnosesb and people living with HIV, compared to other races/ethnicities. In 2017, blacks/African Americans accounted for 13% of the US populationc but 43% (16,694) of the 38,739 new HIV diagnoses in the United States and dependent areas.d
The Numbers
HIV Diagnoses
In 2017:
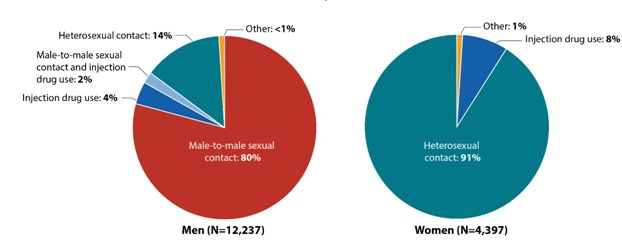
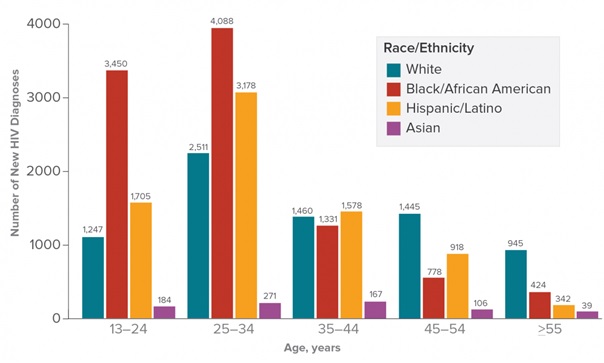
- Seventy-three percent (12,237) of adult and adolescent blacks/African Americans who received an HIV diagnosis were men and 26% (4,397) were women.
- Sixty percent (10,070) of blacks/African Americans who received an HIV diagnosis were gay or bisexual men.e,f
- Among black/African American gay and bisexual men who received an HIV diagnosis, 41% (4,088) were aged 25 to 34.
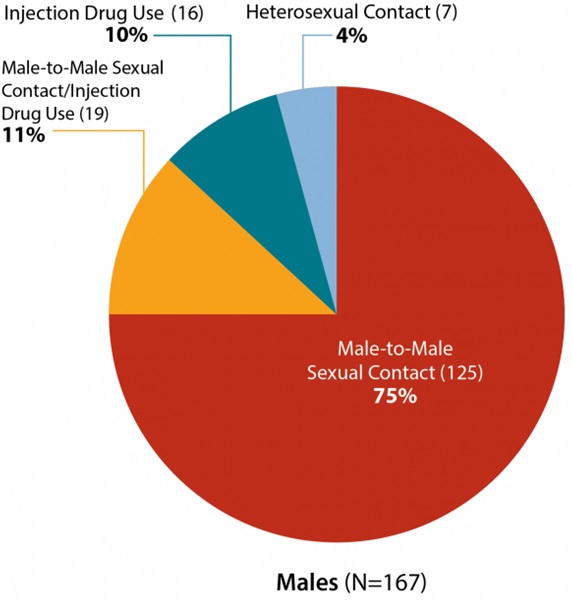
New HIV Diagnoses Among Blacks/African Americans by Transmission Category and Sex in the US and Dependent Areas, 2017
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. New HIV Diagnoses in the US and Dependent Areas for the Most-Affected Subpopulations, 2017
Hispanics/Latinos can be of any race. Subpopulations representing 2% or less of HIV diagnoses are not reflected in this chart. Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. From 2010 to 2016, HIV diagnoses decreased 12% among blacks/African Americans overall in the 50 states and the District of Columbia. But trends varied for different groups of blacks/African Americans. HIV Diagnoses Among Blacks/African Americans in the 50 States and District of Columbia, 2010-2016
CDC. NCHHSTP AtlasPlus. Accessed January 24, 2019 Living With HIV In the 50 states and the District of Columbia: An estimated 468,800 blacks/African Americans had HIV in 2015, representing 42% of all people with HIV.g Of those, an estimated 85% were aware of their infection.
A person with HIV who takes HIV medicine as prescribed and gets and stays virally suppressed or undetectable can stay healthy and has effectively no risk of sexually transmitting HIV to HIV-negative partners. Deaths In 2016, there were 6,804 deaths among blacks/African Americans with diagnosed HIV in the US. These deaths may be due to any cause.
Prevention Challenges
1 in 7 blacks/African Americans with HIV are unaware they have it. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.
Some African American communities have higher rates of some sexually transmitted diseases (STDs) than other racial/ethnic communities. Having another STD can increase a person's chance of getting or transmitting HIV.
Stigma, fear, discrimination, and homophobia may place many African Americans at higher risk for HIV.
The poverty rate is higher among African Americans than other racial/ethnic groups. The socioeconomic issues associated with poverty—including limited access to high-quality health care, housing, and HIV prevention education—directly and indirectly increase the risk for HIV infection and affect the health of people living with and at risk for HIV. These factors may explain why African Americans have worse outcomes on the HIV continuum of care, including lower rates of linkage to care and viral suppression.
What CDC Is Doing CDC funds state and local health departments and community-based organizations (CBOs) to deliver effective HIV prevention services for African Americans. For example:
- Under the new integrated HIV surveillance and prevention cooperative agreement, CDC is awarding around $400 million per year to health departments for surveillance and prevention efforts. This award will direct resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the United States
- In 2019, CDC will award a new cooperative agreement to strengthen the capacity and improve the performance of the nation's HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training and technical assistance tailored within four geographic regions.
- In 2017, CDC awarded nearly $11 million per year for 5 years to 30 CBOs to provide HIV testing to young gay and bisexual men of color and transgender youth of color, with the goals of identifying undiagnosed HIV infections and linking those who have HIV to care and prevention services.
- In 2015, CDC added three awards to help health departments reduce HIV infections and improve engagement and retention in HIV medical care among gay and bisexual men of color.
- Targeted Highly-Effective Interventions to Reverse the HIV Epidemic (THRIVE) supports state and local health department demonstration projects to develop community collaborations that provide comprehensive HIV prevention and care services for gay and bisexual men of color at risk for and living with HIV infection.
- Training and Technical Assistance for THRIVE strengthens the capacity of funded health departments and their collaborative partners to plan, implement, and sustain (through ongoing engagement, assessment, linkage, and retention) comprehensive prevention, care, behavioral health, and social services models for gay and bisexual men of color at risk for and living with HIV infection.
- Project PrIDE (PrEP, Implementation, Data to Care, and Evaluation) supports 12 health departments in implementing PrEP and Data to Care demonstration projects for gay and bisexual men and transgender persons, with a particular emphasis on persons of color.
- Through its Let's Stop HIV Together campaigns and partnerships, CDC provides African Americans with effective and culturally appropriate messages about HIV prevention and treatment. For example,
- Stop HIV Stigma fights stigma among all Americans and provides many stories about people living with HIV.
- Doing It encourages all adults to know their HIV status and protect themselves and their community by making HIV testing a part of their regular health routine.
- Start Talking. Stop HIV. helps gay and bisexual men communicate about testing and a range of HIV prevention strategies.
- HIV Treatment Works shows how people living with HIV have overcome barriers to stay in care and provides resources on how to live well with HIV.
- Partnering and Communicating Together (PACT) to Act Against AIDS, a 5-year partnership with organizations such as the National Black Justice Coalition, the National Urban League, and the Black Men's Xchange, is raising awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including African Americans.
-
- Black refers to people having origins in any of the black racial groups of Africa, including immigrants from the Caribbean, and South and Latin America. African American is a term often used for Americans of African descent with ancestry in North America. Individuals may self-identify as either, both, or choose another identity altogether. This fact sheet uses African American, unless referencing surveillance data.
- HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
- The US Census Bureau's population estimates include the 50 states, the District of Columbia, and Puerto Rico.
- Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
- The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
- Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
- Includes diagnosed and undiagnosed HIV infections among adults and adolescents.
Bibliography
https://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html HIV and African American Gay and Bisexual Men
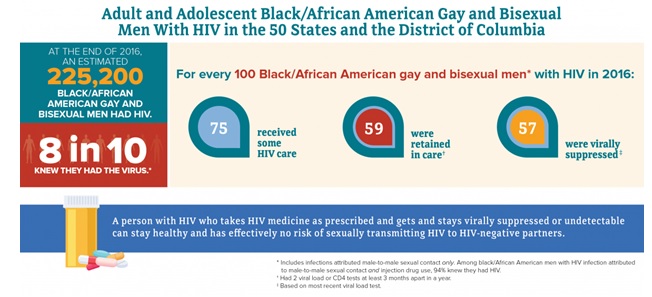
Black/African Americana gay, bisexual, and other men who have sex with menb are more affected by HIV than any other group in the United States. In 2017, black/African American gay and bisexual men accounted for 26% (10,070) of the 38,739 new HIV diagnoses and 37% of new diagnoses among all gay and bisexual men in the United States and dependent areas.c,d
The Numbers
HIV Diagnosese
Prevention Challenges
Stigma, homophobia, and discrimination put gay and bisexual men of all races/ethnicities at risk for multiple physical and mental health problems and affects whether they seek and are able to receive high-quality health services, including HIV testing, treatment, and other prevention services. In addition to stigma and other risk factors affecting all gay and bisexual men, several factors are particularly important for African American gay and bisexual men. These include the following:
Lack of awareness of HIV status. People who don't know they have HIV cannot get the medicine they need to stay healthy and prevent transmitting HIV to their partners. Therefore, they may transmit the infection to others without knowing it.
Timely linkage to HIV medical care. According to a recent MMWR, only 67% of HIV-positive African American gay and bisexual men with newly diagnosed HIV, and 58% with previously diagnosed HIV, were linked to HIV medical care within 90 days of the diagnosis. Early linkage to HIV medical care is essential to achieving viral suppression.
Low percentages of viral suppression. African American gay and bisexual men have lower percentages of viral suppression compared to gay and bisexual men of other races/ethnicities. Because of the low percentages of viral suppression, the higher prevalence of HIV in that population, and the greater likelihood of having sexual partners of the same race, compared with other races/ethnicities, African American gay and bisexual men are at greater risk of being exposed to HIV.
Socioeconomic factors. The poverty rate is higher among African Americans than other racial/ethnic groups. The socioeconomic issues associated with poverty—including limited access to high-quality health care, housing, and HIV prevention education—directly and indirectly increase the risk of HIV infection for some African American gay and bisexual men and may also affect the health of people who have HIV.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies among African American gay and bisexual men. Funding state, territorial, and local health departments is CDC's largest investment in HIV prevention.
- Under the strategic partnerships and planning cooperative agreement, CDC will fund a national organization to support integrated HIV programs through the development of strategic national partnerships and enhanced communication efforts. This funding opportunity will also provide funding to health departments to engage community partners in a planning process to help develop jurisdictional Ending the HIV Epidemic plans.
- In 2017, CDC awarded nearly $11 million per year for 5 years to 30 CBOs to provide HIV testing to young gay and bisexual men of color and transgender youth of color, with the goals of identifying undiagnosed HIV infections and linking those who have HIV to care and prevention services.
- Under the integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for HIV data collection and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the US.
- In 2019, CDC awarded a cooperative agreement to strengthen the capacity and improve the performance of the nation's HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions.
- Under the flagship community-based organization cooperative agreement, CDC awarded about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to people at greatest risk.
- Through its Let's Stop HIV Together (formerly Act Against AIDS) campaign, CDC provides African American gay and bisexual men with effective and culturally appropriate messages about HIV testing, prevention, and treatment. For example,
- Stop HIV Stigma highlights the role that each person plays in stopping HIV stigma and gives voice to people living with HIV, as well as their friends and family.
- Doing It motivates all adults to get tested for HIV and know their status.
- Start Talking. Stop HIV. focuses on gay and bisexual men and encourages open communication between sex partners and friends about HIV prevention strategies.
- HIV Treatment Works shows how people with HIV have been successful getting care and staying on treatment.
- Partnering and Communicating Together (PACT raises awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including African American gay and bisexual men.
To learn more about a range of health issues affecting African American gay and bisexual men, visit the CDC Gay and Bisexual Men's Health site.
- Black refers to people having origins in any of the black racial groups of Africa, including immigrants from the Caribbean, and South and Latin America. African American is a term often used for Americans of African descent with ancestry in North America. Individuals may self-identify as either, both, or choose another identity altogether. This fact sheet uses African American, unless referencing surveillance data.
- The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
- Unless otherwise noted, the term United States includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
- Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
- HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
Bibliography
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
- CDC. Estimated incidence and prevalence in the United States 2010-2016. HIV Surveillance Supplemental Report 2018;23(1).
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2017. HIV Surveillance Supplemental Report 2019;24(3).
- CDC. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 20 U.S. cities, 2014. HIV Surveillance Special Report 2016;15.
- CDC. HIV surveillance—Men who have sex with men (slides). Accessed July 24, 2019.
- CDC. High-impact HIV prevention: CDC's approach to reducing HIV infections in the United States. Accessed July 24, 2019.
- CDC. HIV care outcomes among men who have sex with men with diagnosed HIV infection—United States, 2015. MMWR 2017;66(37):969-74.
- Marano M, Stein R, Song W, et al. HIV testing, linkage to HIV medical care, and interviews for partners services among black men who have sex with men—non-health care facilities, 20 southern U.S. jurisdictions, 2016. MMWR 2018;67(28):778-81.
https://www.cdc.gov/hiv/group/msm/bmsm.html HIV and American Indians and Alaska Natives American Indians and Alaska Natives (AI/AN) represent about 1.3%a of the U.S. population. Overall, diagnosed HIV infections among AI/AN are proportional to their population size, but HIV diagnoses have increased over time. The Numbers HIV and AIDS Diagnoses
HIV Diagnoses Among American Indians/Alaska Natives in the US and Dependent Areas by Transmission Category and Sex, 2017c
The terms male-to-male sexual contact and male-to-male sexual contact and injection drug use are used in the CDC surveillance systems. They indicate the behaviors that transmit HIV infection, not how individuals self-identify in terms of their sexuality. Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
- Of the 38,739 HIV diagnoses in the United States in 2017, 1% (212) were among AI/AN.
- From 2010 to 2016, the annual number of HIV diagnoses increased 46% (from 157 to 230) among AI/AN overall and 81% (from 90 to 163) among AI/AN gay and bisexual men.
Living With HIV and Deaths
- An estimated 3,600 AI/AN had HIV in 2016 and 82% of them had received a diagnosis.
- Of AI/AN with HIV in 2015, 60% received HIV care, 43% were retained in care, and 48% had achieved viral suppression.e
- During 2016, 46 AI/AN with diagnosed HIV died in the US. These deaths may be due to any cause.
A person with HIV who takes HIV medicine as prescribed and gets and stays virally suppressed or undetectable can stay healthy and has effectively no risk of sexually transmitting HIV to HIV-negative partners.
Prevention Challenges
- Sexually transmitted diseases (STDs). From 2013 to 2017, AI/AN had the second highest rates of chlamydia and gonorrhea among all racial/ethnic groups. Having another STD increases a person's risk for getting or transmitting HIV.
- Awareness of HIV status. An estimated 8 in 10 AI/AN with HIV in 2016 had received a diagnosis. It is important for everyone to know their HIV status. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.
- Cultural stigma and confidentiality concerns. AI/AN gay and bisexual men may face culturally based stigma and confidentiality concerns that could limit opportunities for education and HIV testing, especially among those who live in rural communities or on reservations.
- Cultural diversity. There are over 560 federally recognized AI/AN tribes, whose members speak over 170 languages. Because each tribe has its own culture, beliefs, and practices, creating culturally appropriate prevention programs for each group can be challenging.
- Socioeconomic issues. Poverty, including limited access to high-quality housing, directly and indirectly increases the risk for HIV infection and affects the health of people who have and are at risk for HIV infection. Compared with other racial/ethnic groups, AI/AN have higher poverty rates, have completed fewer years of education, are younger, are less likely to be employed, and have lower rates of health insurance coverage.
- Alcohol and illicit drug use. Alcohol and substance use can impair judgment and lead to behaviors that increase the risk of HIV. Injection drug use can directly increase the risk of HIV through sharing contaminated needles, syringes, and other equipment. Compared with other racial/ethnic groups, AI/AN tend to use alcohol and drugs at a younger age and use them more often and in higher quantities.
- Data limitations. Racial misidentification of AI/AN may lead to the undercounting of this population in HIV surveillance systems and may contribute to the underfunding of targeted services for AI/AN.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention methods and improve HIV data collection among AI/AN. Activities include:
- Under the new integrated HIV surveillance and prevention cooperative agreement, CDC is awarding around $400 million per year to health departments for surveillance and prevention efforts. This award will direct resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the United States.
- In 2019, CDC will award a new cooperative agreement to strengthen the capacity and improve the performance of the nation's HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training and technical assistance tailored within four geographic regions.
- Ensuring that capacity-building assistance providers incorporate cultural competency, linguistics, and educational appropriateness into all services delivered.
- Through its Let's Stop HIV Together(formerly Act Against AIDS) campaigns and partnerships, CDC provides effective and culturally appropriate messages aimed at stopping HIV stigma and promoting HIV testing, prevention, and treatment. The stigma materials include stories and issues relevant to AI/AN, as do the following:
- Doing It encourages all people to know their HIV status and protect themselves and their community by making HIV testing a part of their regular health routine.
- Start Talking. Stop HIV. helps gay and bisexual men communicate about testing and a range of HIV prevention strategies.
- HIV Treatment Works shows how people living with HIV have overcome barriers to stay in care and provides resources on how to live well with HIV.
- Partnering and Communicating Together (PACT) to Act Against AIDS, a 5-year partnership with organizations such as the ASPIRA Association and AIDS United, is raising awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including AI/AN.
In addition, the Office for State, Tribal, Local, and Territorial Support (OSTLTS) serves as the primary link between CDC, the Agency for Toxic Substance and Disease Registry, and tribal governments. OSTLTS's tribal support activities are focused on fulfilling CDC's supportive role in ensuring that AI/AN communities receive public health services that keep them safe and healthy.
- Percentage of AI/AN reporting only one race. The US Census Bureau's population estimates include the 50 states, the District of Columbia, and Puerto Rico.
- HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
- Unless otherwise noted, the term United States includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
- Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
- People are considered retained in care if they get two viral load or CD4 tests at least 3 months apart in a year. (CD4 cells are the cells in the body's immune system that are destroyed by HIV.) Viral suppression is based on the most recent viral load test.
Bibliography
- CDC. Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report2019;24(1).
- US Census Bureau. QuickFacts United States: American Indians and Alaska Natives. Accessed February 5, 2019.
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. Accessed February 5, 2019.
- CDC. NCHHSTP AtlasPlus. Accessed February 21, 2019.
- CDC. High-impact HIV prevention: CDC's approach to reducing HIV infections in the United States. Accessed February 5, 2019.
- CDC. Improving HIV surveillance among American Indians and Alaska Natives in the United States( https://www.cdc.gov/hiv/pdf/policies_strategy_nhas_native_americans.pdf). Accessed February 5, 2019.
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2015. HIV Surveillance Supplemental Report 2017;22(2). Accessed February 5, 2019.
- CDC. Selected national HIV prevention and care outcomes (slides). Accessed February 5, 2019.
- CDC. Sexually transmitted disease surveillance 2017 (slides). Accessed February 5, 2019.
- Burks DJ, Robbins R, Durtschi JP. American Indian gay, bisexual and two-spirit men: A rapid assessment of HIV/AIDS risk factors, barriers to prevention and culturally-sensitive intervention. Cult Health Sex 2011;13(3):283-98. PubMed Abstract.
- Bureau of Indian Affairs. Indian entities recognized and eligible to receive services from the United States Bureau of Indian Affairs. Fed Regist 2012;77(155):47868. Accessed February 5, 2019.
- James C, Schwartz K, Berndt J. A profile of American Indians and Alaska Natives and their health coverage. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2009. Accessed February 5, 2019.
- Walters KL, Simoni JM, Evans-Campbell T. Substance use among American Indians and Alaska Natives: Incorporating culture in an ‘Indigenist' stress-coping paradigm. Public Health Rep 2002;117(1):s104-17. PubMed Abstract.
- Bertolli J, Lee LM, Sullivan PS, American Indian/Alaska Native Race/Ethnicity Data Validation Workgroup. Racial misidentification of American Indians/Alaska Natives in the HIV/AIDS reporting systems of five states and one urban health jurisdiction, US, 1984–2000. Public Health Rep 2007;122(3):382-94. PubMed Abstract.
- CDC. Deaths: Final data for 2015. National Vital Statistics Reports 2017; 66(6). Accessed January 26, 2018.
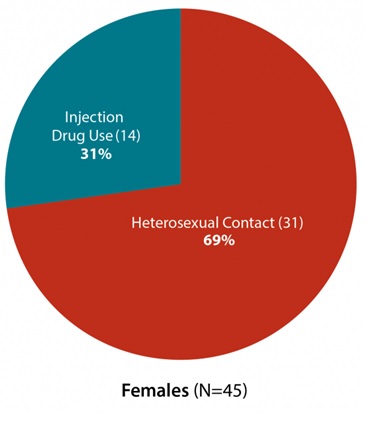
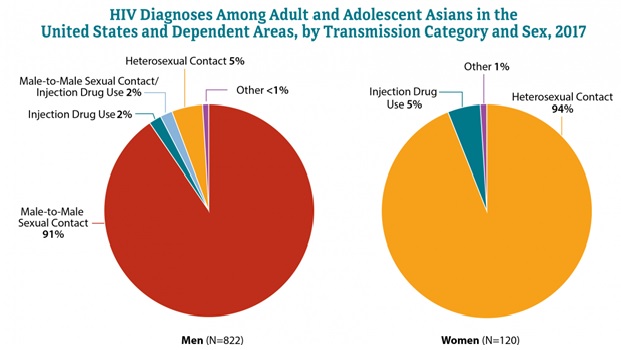
https://www.cdc.gov/hiv/group/racialethnic/aian/index.html HIV and Asians Between 2010 and 2016 the Asian population (a) in the United States grew around 17%, four times as fast as the total US population.b During the same period, in the 50 states and the District of Columbia, the number of Asians receiving an HIV diagnosis increased by 42%, driven primarily by an increase in HIV diagnoses among Asian gay and bisexual men.c Asians, who make up 6% of the population, accounted for about 2% of HIV diagnoses in 2017 in the United States and dependent areas.(d) The NumbersHIV Diagnoses
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
From 2010 to 2016, annual HIV diagnoses in the 50 states and the District of Columbia increased by 52% among Asian gay and bisexual men.(f)
Living With HIV and Deaths
During 2016, there were 95 deaths among Asians with diagnosed HIV in the US and dependent areas. These deaths may be due to any cause
Prevention Challenges
There are some behaviors that put everyone at risk for HIV. These include having anal or vaginal sex without protection (like a condom or medicine to prevent or treat HIV) or sharing injection drug equipment with someone who has HIV. Other factors that affect Asians particularly include:
- Undiagnosed HIV. People with undiagnosed HIV cannot obtain the care they need to stay healthy and may unknowingly transmit HIV to others. A lower percentage of Asians with HIV have received a diagnosis, compared to other races/ethnicities.
- Cultural factors. Some Asians may avoid seeking testing, counseling, or treatment because of language barriers or fear of discrimination, the stigma of homosexuality, immigration issues, or fear of bringing shame to their families.
- Limited research. Limited research about Asian health and HIV infection means there are few targeted prevention programs and behavioral interventions for this population.
- Data limitations. The reported number of HIV cases among Asians may not reflect the true HIV diagnoses in this population because of race/ethnicity misidentification. This could lead to the underestimation of HIV infection in this population.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies and improve surveillance among Asians. Funding state, territorial, and local health departments is CDC's largest investment in HIV prevention.
- Under the new integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for surveillance and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the United States.
- In 2019, CDC awarded a new cooperative agreement to strengthen the capacity and improve the performance of the nation's HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions. The Asian and Pacific Islander American Health Forum is funded under this effort.
- Under the flagship community-based organization cooperative agreement, CDC awarded about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to people at greatest risk. Special Service for Groups/APAIT is funded under this effort.
- The CDC publication, Effective HIV Surveillance Among Asian Americans and Native Hawaiians and Other Pacific Islanders, provides recommendations for improving HIV surveillance activities for health departments in states with high concentrations of Asians and NHOPIs. CDC continues to collect and report data for Asian and NHOPI populations separately in annual, supplemental, and special surveillance reports and annual program monitoring reports.
- Through its Let's Stop HIV Together (formerly Act Against AIDS) campaigns and partnerships, CDC provides Asians with effective and culturally appropriate messages aimed at stopping HIV stigma and promoting HIV testing, prevention, and treatment. The stigma materials include stories and issues relevant to Asians, as do the following:
- Doing It encourages all people to know their HIV status and protect themselves and their community by making HIV testing a part of their regular health routine.
- Start Talking. Stop HIV. helps gay and bisexual men communicate about testing and a range of HIV prevention strategies.
- HIV Treatment Works shows how people living with HIV have overcome barriers to stay in care and provides resources on how to live well with HIV.
- Partnering and Communicating Together (PACT) to Act Against AIDS is raising awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including Asians.
- A person having origins in any of the original peoples of the Far East, Southeast Asia, or the Indian subcontinent including, for example, Cambodia, China, India, Japan, Korea, Malaysia, Pakistan, the Philippine Islands, Thailand, and Vietnam.
- The US Census Bureau's population estimates include the 50 states, the District of Columbia, and Puerto Rico.
- Male-to-male sexual contact is the term used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
- American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
- Diagnoses includes the number of people receiving an HIV diagnosis each year (regardless of the year they were infected).
- Includes infections attributed to male-to-male sexual contact and injection drug use (men who reported both risk factors).
Bibliography
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. Accessed March 8, 2019.
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2016. HIV Surveillance Supplemental Report 2016;23(4). Accessed March 8, 2019.
- CDC. Estimated HIV incidence and prevalence in the United States 2010–2016. HIV Surveillance Supplemental Report. 2018;24. Accessed March 8, 2019.
- CDC. Selected national HIV prevention and care outcomes [slide set]. Accessed March 8, 2019.
- CDC. High-Impact HIV prevention: CDC's approach to reducing HIV infections in the United States. Accessed March 8, 2019.
- CDC. NCHHSTP atlas plus. Accessed March 8, 2019.
- CDC. Effective HIV surveillance among Asian Americans and other Pacific Islanders. Accessed March 8, 2019.
- Hahm HC, Lee J, Rough K, Strathdee SA. Gender power control, sexual experiences, safer sex practices, and potential HIV risk behaviors among Asian-American women. AIDS Behav 2012;16(1):179-88.
- Russ LW, Meyer AC, Takahashi LM, et al. Examining barriers to care: provider and client perspectives on the stigmatization of HIV-positive Asian-Americans with or without viral hepatitis co-infection. AIDS Care 2012;24(10):1302-7.
- US Census Bureau. QuickFacts: United States. Accessed March 8, 2019.
https://www.cdc.gov/hiv/group/racialethnic/asians/index.htmlHIV and Hispanics/Latinos
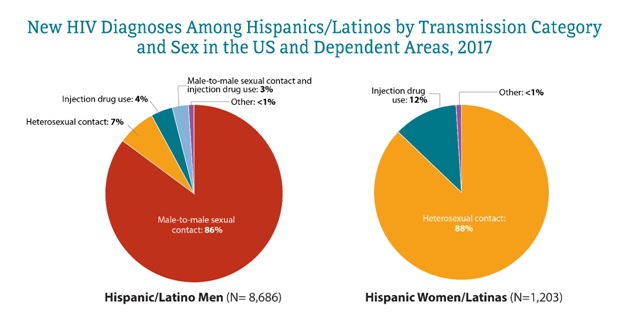
HIV continues to be a serious threat to the health of Hispanic/Latinoa communities. In 2017, adult and adolescent Hispanics/Latinos made up 26% (9,889) of the 38,739 new HIV diagnosesb in the United States (US) and dependent areas.(c)
The Numbers
HIV Diagnoses
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
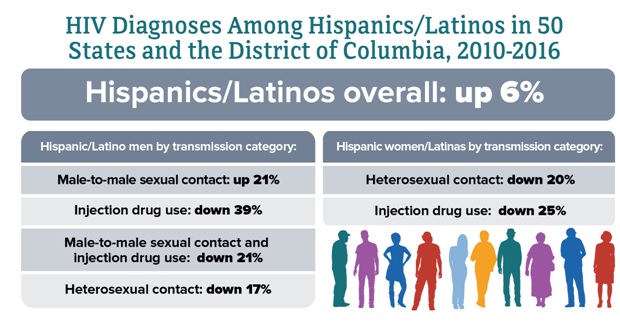
Subpopulations representing 2% or less of HIV diagnoses are not reflected in this chart. Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. From 2010 to 2016, HIV diagnoses increased 6% among Hispanics/Latinos overall in 50 states and the District of Columbia. But trends varied by transmission category.
Source: CDC. NCHHSTP AtlasPlus. Accessed October 8, 2019.
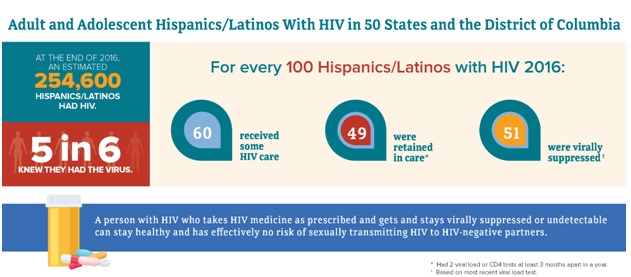
Living With HIV
Sources: CDC. Estimated HIV incidence and prevalence in the United States 2010–2016. HIV Surveillance Supplemental Report. 2018;24(1). CDC. NCHHSTP AtlasPlus. Accessed October 8, 2019. Deaths In 2016, there were 2,863 deaths among Hispanics/Latinos with diagnosed HIV in the US and dependent areas. These deaths may be due to any cause.
Prevention Challenges
- 1 in 6 Hispanics/Latinos with HIV are unaware they have it. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.
- Hispanics/Latinos have higher rates of some sexually transmitted diseases (STDs) than some other races/ethnicities. Having another STD can increase a person's chance of getting or transmitting HIV.
- Poverty, migration patterns, lower educational level, and language barriers may make it harder for some Hispanics/Latinos to get HIV testing and care.
- Some Hispanics/Latinos may not use HIV prevention services, get an HIV test, or get treatment if they have HIV due to fear of disclosing their immigration status.
- Hispanics/Latinos experience high levels of mistrust of the health care system. Lower levels of trust can reduce the likelihood of clinic visits and result in lower use of and adherence to antiretroviral medications.
- Though not unique to Hispanics/Latinos, stigma, fear, discrimination, and homophobia may impact the lives of some Hispanics/Latinos. These issues may put some Hispanics/Latinos at higher risk for HIV infection.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies among Hispanics/Latinos. Funding state, territorial, and local health departments is CDC's largest investment in HIV prevention.
- Under the strategic partnerships and planning cooperative agreement, CDC will fund a national organization to support integrated HIV programs through the development of national partnerships and enhanced communication efforts. This funding opportunity will also provide funding to health departments to engage community partners in a planning process to help develop jurisdictional Ending the HIV Epidemic plans.
- Under the integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for HIV data collection and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the US.
- In 2019, CDC awarded a cooperative agreement to strengthen the capacity and improve the performance of the nation's HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions.
- In 2017, CDC awarded nearly $11 million per year for 5 years to 30 CBOs to provide HIV testing to young gay and bisexual men of color and transgender youth of color, with the goals of identifying undiagnosed HIV infections and linking those who have HIV to care and prevention services.
- CDC is funding a demonstration project in 4 jurisdictions to identify active HIV transmission networks and implement HIV interventions for Hispanic/Latino gay, bisexual, and other men who have sex with men. Activities include assessing transmission and risk networks, HIV testing, and linking people with HIV to care and treatment.
- Under the flagship community-based organization cooperative agreement, CDC awarded about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to key populations.
- Through its Let's Stop HIV Together campaign (formerly Act Against AIDS), CDC provides Hispanics/Latinos with culturally and linguistically appropriate messages about HIV testing, prevention, and treatment. For example,
- Stop HIV Stigma highlights the role that each person plays in stopping HIV stigma and gives voice to people living with HIV, as well as their friends and family.
- Doing It motivates all adults to get tested for HIV and know their status.
- Start Talking. Stop HIV. focuses on gay and bisexual men and encourages open communication between sex partners and friends about HIV prevention strategies.
- HIV Treatment Works shows how people with HIV have been successful getting care and staying on treatment.
- Partnering and Communicating Together (PACT) raises awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including Hispanics/Latinos.
- Hispanics/Latinos can be of any race.
- HIV diagnoses refers to the number of people who received a diagnosis of HIV during a given time period, not when the people got HIV infection.
- Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
Bibliography
HIV and Native Hawaiians and Other Pacific Islanders
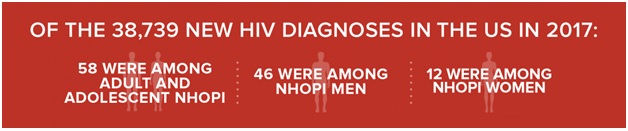
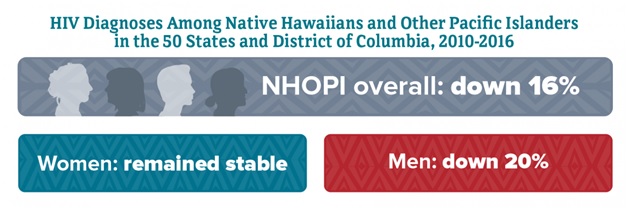
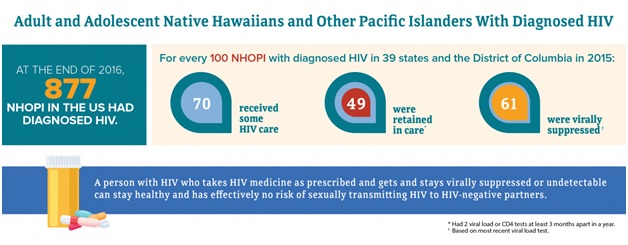
Although Native Hawaiians and Other Pacific Islanders (NHOPI) account for a very small percentage of new HIV diagnosesa in the United States (US) and dependent areas,b HIV affects NHOPI in ways that are not always apparent because of their small population sizes. In 2017, NHOPI made up 0.2% of the US population.c The Numbers
HIV Diagnoses
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. From 2010 to 2016, HIV diagnoses decreased 16% among NHOPI overall in the 50 states and the District of Columbia. But trends varied by gender
Living With HIV
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29. CDC. Selected national HIV prevention and care outcomes (slides). Accessed April 25, 2019. Deaths In 2016, there were 14 deaths among adult and adolescent NHOPI with diagnosed HIV in the US and dependent areas. These deaths may be due to any cause.
Prevention Challenges
There are some behaviors that put everyone at risk for HIV. These behaviors include having anal or vaginal sex without protection (like a condom or medicine to prevent or treat HIV), or sharing injection drug equipment with someone who has HIV. Factors that particularly affect NHOPI include:
- Socioeconomic factors. Poverty, inadequate or no health care coverage, language barriers, and lower educational attainment among NHOPI may contribute to lack of awareness about HIV risk and higher-risk behaviors.
- Cultural factors. NHOPI cultural customs, such as not talking about sex across generations, may stigmatize sexuality in general, and homosexuality specifically, as well as interfere with HIV risk-reduction strategies, such as condom use.
- Limited research. Limited research about NHOPI health and HIV infection and small population numbers have resulted in a lack of targeted prevention programs and behavioral interventions for this population.
- Data limitations. The low reported number of HIV cases among NHOPI may not reflect the true burden of HIV in this population because of race/ethnicity misidentification. This could lead to an underestimation of HIV infection in this population.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies and improve surveillance among NHOPI. Funding state, territorial, and local health departments is CDC's largest investment in HIV prevention.
- Under the new integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for surveillance and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the United States.
- In 2019, CDC awarded a new cooperative agreement to strengthen the capacity and improve the performance of the nation's HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions. The Asian and Pacific Islander American Health Forum is funded under this effort.
- Under the flagship community-based organization cooperative agreement, CDC awarded about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to people at greatest risk. Special Service for Groups/APAIT is funded under this effort.
- The CDC publication Effective HIV Surveillance Among Asian Americans and Native Hawaiians and Other Pacific Islanders provides recommendations for improving HIV surveillance activities for health departments in states with high concentrations of Asians and NHOPIs. CDC continues to collect and report data for Asian and NHOPI populations separately in annual, supplemental, and special surveillance reports and annual program monitoring reports.
- Through its Let's Stop HIV Together (formerly Act Against AIDS) campaigns and partnerships, CDC provides NHOPI with effective and culturally appropriate messages aimed at stopping HIV stigma and promoting HIV testing, prevention, and treatment. The stigma materials include stories and issues relevant to NHOPI, as do the following:
- Doing It encourages all people to know their HIV status and protect themselves and their community by making HIV testing a part of their regular health routine.
- Start Talking. Stop HIV. helps gay and bisexual men communicate about testing and a range of HIV prevention strategies.
- HIV Treatment Works shows how people living with HIV have overcome barriers to stay in care and provides resources on how to live well with HIV.
- Partnering and Communicating Together (PACT) to Act Against AIDS is raising awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including NHOPI.
- HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
- Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
- The US Census Bureau's population estimates include the 50 states, the District of Columbia, and Puerto Rico.
Bibliography
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
- CDC. Estimated HIV incidence and prevalence in the United States 2010-2016. HIV Surveillance Supplemental Report 2019;24(1).
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2016. HIV Surveillance Supplemental Report 2018;23(4).
- CDC. NCHHSTP AtlasPlus. Accessed April 25, 2019.
- CDC. Selected national HIV prevention and care outcomes (slides).
- Adih WK, Campsmith M, Williams CL, Hardnett FP, Hughes D. Epidemiology of HIV among Asians and Pacific Islanders in the United States, 2001-2008. J Int Assoc Physicians AIDS Care (Chic) 2011;10(3):150-9. PubMed abstract.
- DiStefano AS, Hui B, Barrera-Ng A, et al. Contextualization of HIV and HPV risk and prevention among Pacific Islander young adults in Southern California. Soc Sci Med 2012;75(4):699-708. PubMed abstract.
- Takahashi LM, Kim AJ, Sablan-Santos L, et al. HIV testing behavior among Pacific Islanders in Southern California: Exploring the importance of race/ethnicity, knowledge, and domestic violence. AIDS Educ Prev 2011;23(1):54-64. PubMed abstract.
https://www.cdc.gov/hiv/group/racialethnic/nhopi/index.html
C. History
1. HIV and AIDS Timeline
A Timeline of HIV/AIDS The HIV.gov Timeline reflects the history of the domestic HIV/AIDS epidemic from the first reported cases in 1981 to the present—where advances in HIV prevention, care, and treatment offer hope for a long, healthy life to people who are living with, or at risk for, HIV and AIDS.
1981
- June 5: The U.S. Centers for Disease Control and Prevention (CDC) publish a Morbidity and Mortality Weekly Report (MMWR), describing cases of a rare lung infection, Pneumocystis carinii pneumonia (PCP), in five young, previously healthy, gay men in Los Angeles. All the men have other unusual infections as well, indicating that their immune systems are not working; two have already died by the time the report is published. This edition of the MMWR marks the first official reporting of what will become known as the AIDS epidemic.
- June 5-6: The Associated Press, the Los Angeles Times, and the San Francisco Chronicle report on the MMWR article. Within days, CDC receives numerous reports of similar cases of PCP and other opportunistic infections among gay men—including reports of a cluster of cases of a rare, and unusually aggressive, cancer, Kaposi's Sarcoma (KS), among a group of gay men in New York and California.
- June 8: In response to these reports, CDC establishes the Task Force on Kaposi's Sarcoma and Opportunistic Infections to identify risk factors and to develop a case definition for national surveillance.
- July 3: CDC releases another MMWR on KS and PCP among 26 gay men in New York and California. On the same day, the New York Times publishes an article entitled “Rare Cancer Seen in 41 Homosexuals.” At this point, the term “gay cancer” enters the public lexicon.
- September 21: The nation's first Kaposi's Sarcoma clinic opens at the University of California, San Francisco Medical Center.
- December 10: Bobbi Campbell, a San Francisco nurse, becomes the first KS patient to go public. Calling himself the “KS Poster Boy,“ Campbell writes a newspaper column on living with “gay cancer” for the San Francisco Sentinel. He also posts photos of his lesions in the window of a local drugstore to alert the community to the disease and encourage people to seek treatment.
- By year's end, there is a cumulative total of 270 reported cases of severe immune deficiency among gay men, and 121 of those individuals have died. Some researchers begin calling the condition GRID (Gay-Related Immune Deficiency). This terminology influences both the medical profession and the public to perceive the epidemic as limited to gay men, with serious long-term consequences for women, heterosexual men, hemophiliacs, people who inject drugs, and children.
1982
- January 4: Gay Men's Health Crisis, the first community-based AIDS service provider in the U.S., is founded in New York City.
- April 13: U.S. Representative Henry Waxman convenes the first congressional hearings on AIDS at the Los Angeles Gay and Lesbian Community Services Center in Hollywood, California. At the hearing, Dr. James Curran, head of the CDC's Task Force on Kaposi's Sarcoma and Opportunistic Infections, estimates that tens of thousands of people may be affected by the disease.
- May 9: The Kaposi's Sarcoma (KS) Research and Education Foundation is formed to provide information on KS to gay men in San Francisco. The organization will ultimately become the San Francisco AIDS Foundation.
- September 24: CDC uses the term “AIDS” (Acquired Immune Deficiency Syndrome) for the first time, and releases the first case definition of AIDS: “a disease at least moderately predictive of a defect in cell-mediated immunity, occurring in a person with no known case for diminished resistance to that disease.”
- September 24: Rep. Waxman and Rep. Phillip Burton introduce legislation to allocate $5 million to CDC for surveillance and $10 million to the National Institutes of Health (NIH) for AIDS research.
- December 10: CDC reports a case of AIDS in an infant who received blood transfusions. The following week, the MMWR reports 22 cases of unexplained immunodeficiency and opportunistic infections in infants.
1983
- January 1: Ward 86, the world's first dedicated outpatient AIDS clinic, opens at San Francisco General Hospital.
- January 4: CDC hosts a public meeting with the representatives from the U.S. Food and Drug Administration (FDA), NIH, the blood services community, gay activists, and hemophilia specialists to identify opportunities to protect the nation's blood supply from AIDS, but participants fail to reach consensus on appropriate action.
- January 7: CDC reports cases of AIDS in female sexual partners of males with AIDS.
- In February, CDC establishes the National AIDS Hotline to respond to public inquiries about the disease.
- In the March 4 edition of the Morbidity and Mortality Weekly Report (MMWR), CDC notes that most cases of AIDS have been reported among homosexual men with multiple sexual partners, people who inject drugs, Haitians, and hemophiliacs. The report suggests that AIDS may be caused by an infectious agent that is transmitted sexually or through exposure to blood or blood products and issues recommendations for preventing transmission.
- May 18: The U.S. Congress passes the first bill that includes funding specifically targeted for AIDS research and treatment—$12 million for agencies within the U.S. Department of Health and Human Services (HHS).
- May 20: Dr. Françoise Barré-Sinoussi and her colleagues at the Pasteur Institute in France report the discovery of a retrovirus they call Lymphadenopathy Associated Virus (LAV ) that could be the cause of AIDS.
- In June, people living with AIDS (PLWAs) take over the plenary stage at the National AIDS Forum in Denver, and issue a statement on the right of PLWAs to be at the table when policy is made, to be treated with dignity, and to be called “people with AIDS,” not “AIDS victims.” The statement becomes known as The Denver Principles [PDF, 19 KB], and it serves as the charter for the founding of the National Association of People with AIDS.
- July 25: San Francisco General Hospital opens Ward 5B, the first dedicated AIDS ward in the U.S. It is fully occupied within days. The ward offers compassionate, holistic care for AIDS patients, and all staff in the ward—from nurses to janitors—have volunteered to work there. This becomes known as the “San Francisco model of care” for HIV-positive patients.
- August 1-2: The U.S. House of Representatives Subcommittee on Government Operations holds hearings on the federal response to AIDS.
- August 8: AIDS activist Bobbi Campbell appears with his partner, Bobby Hilliard, on the cover of Newsweek magazine for the story, “Gay America: Sex, Politics, and the Impact of AIDS.” It is the first time two gay men are pictured embracing one another on the cover of a U.S. mainstream national magazine.
- September 2: In response to growing concerns about the potential for transmission of AIDS in healthcare settings, CDC publishes the first set of occupational exposure precautions for healthcare workers and allied health professionals.
- In the September 9 MMWR, CDC identifies all major routes of HIV transmission—and rules out transmission by casual contact, food, water, air, or environmental surfaces.
- September 30: After a New York doctor is threatened with eviction from his building for treating AIDS patients, the state's Attorney General and Lambda Legal file the first AIDS discrimination lawsuit.
- November 22: The World Health Organization ( WHO) holds its first meeting to assess the global AIDS situation and begins international surveillance.
1984
- Community-based AIDS service organizations join together to form AIDS Action, a national organization in Washington, DC, to advocate on behalf of people and communities affected by the epidemic, to educate the federal government, and to help shape AIDS-related policy and legislation.
- April 23: HHS Secretary Margaret Heckler announces that Dr. Robert Gallo and his colleagues at the National Cancer Institute have found the cause of AIDS, a retrovirus they have labeled HTLV-III. Heckler also announces the development of a diagnostic blood test to identify HTLV-III and expresses hope that a vaccine against AIDS will be produced within two years.
- July 13: CDC states that avoiding injection drug use and reducing needle-sharing “should also be effective in preventing transmission of the virus.”
- August 15: AIDS activist Bobbi Campbell dies of AIDS-related illness at age 32.
- In October, San Francisco officials order bathhouses closed due to high-risk sexual activity occurring in these venues. New York follows suit within a year.
1985
- January 11: CDC revises the AIDS case definition to note that AIDS is caused by a newly identified virus and issue provisional guidelines for blood screening.
- March 2: FDA licenses the first commercial blood test, ELISA, to detect HIV. Blood banks begin screening the U.S. blood supply.
- April 15–17: HHS and WHO host the first International AIDS Conference in Atlanta, Georgia.
- August 27: Ryan White, an Indiana teenager who contracted AIDS through contaminated blood products used to treat his hemophilia, is refused entry to his middle school. His family's protracted legal battles to protect Ryan's right to attend school call national attention to the issue of AIDS, and Ryan chooses to speak out publicly on the need for AIDS education.
- August 31: The Pentagon announces that, beginning October 1, it will begin testing all new military recruits for HIV infection and will reject those who test positive for the virus.
- September 17: President Ronald Reagan mentions AIDS publicly for the first time, calling AIDS “a top priority” and defending his administration against criticisms that funding for AIDS research is inadequate.
- October 2: The U.S. Congress allocates nearly $190 million for AIDS research—an increase of $70 million over the Administration's budget request. The House Appropriations Committee also urges President Reagan to appoint an “AIDS czar.”
- October 2: Actor Rock Hudson dies of AIDS-related illness at age 59. He is the first major U.S. public figure to acknowledge that he has AIDS, and his death marks a turning point in public perceptions about the epidemic. Hudson leaves $250,000 to help set up the American Foundation for AIDS Research (amfAR). Actress Elizabeth Taylor serves as the organization's founding National Chairman.
- December 6: The U.S. Public Health Service issues the first recommendations for preventing HIV transmission from mother to child.
- By year's end, at least one HIV case has been reported from each region of the world [PDF, 49 KB].
1986
- The Robert Wood Johnson Foundation creates the “AIDS Health Services Program” [PDF, 244 KB], providing joint funding with the U.S. Health Resources and Services Administration (HRSA) for demonstration projects in hard-hit U.S. cities. This program serves as a precursor to the Ryan White CARE Act.
- The International Steering Committee for People with HIV/AIDS is created. Six years later, this will become the GNP (Global Network of People Living with HIV/AIDS).
- In May, the International Committee on the Taxonomy of Viruses declares that the virus that causes AIDS will officially be known as Human Immunodeficiency Virus (HIV ).
- July 18: At the National Conference on AIDS in the Black Community in Washington, DC, a group of minority leaders meets with the U.S. Surgeon General, Dr. C. Everett Koop, to discuss concerns about HIV/AIDS in communities of color. This meeting marks the unofficial founding of the National Minority AIDS Council (NMAC).
- October 22: Dr. Koop issues the Surgeon General's Report on AIDS [PDF, 1.98 MB]. The report makes it clear that HIV cannot be spread casually and calls for: a nationwide education campaign (including early sex education in schools); increased use of condoms; and voluntary HIV testing.
- October 24: CDC reports that AIDS cases are disproportionately affecting African-Americans and Latinos. This is particularly true for African- American and Latino children, who make up 90% of perinatally acquired AIDS cases.
- October 29: The Institute of Medicine (IOM), the principal health unit of the National Academy of Sciences, issues a report, Confronting AIDS: Directions for Public Health, Health Care, and Research. The report calls for a “massive media, educational and public health campaign to curb the spread of the HIV infection,” as well as for the creation of a National Commission on AIDS. The IOM estimates that the effort will require a $2 billion investment in research and patient care by the end of the decade.
1987
- In February, AIDS activist Cleve Jones creates the nongovernmental organizations; and champion the first panel of the AIDS Memorial Quilt. rights of those living with HIV.
- February 1: WHO launches The Global Program on • February 4: Emmy-award winning pianist Liberace AIDS to: raise awareness; formulate evidence-based dies of AIDS-related illness at age 67. policies; provide technical and financial support to • In March, playwright and AIDS activist Larry Kramer countries; initiate relevant social, behavioral, and founds ACT UP (the AIDS Coalition to Unleash Power) biomedical research; promote participation by in New York City.
- March 19: FDA approves the first antiretroviral drug, zidovudine (AZT ). The U.S. Congress approves $30 million in emergency funding to states for AZT—laying the groundwork for what will be the AIDS Drug Assistance Program (ADAP), authorized by the Ryan White CARE Act in 1990.
- March 19: FDA issues regulations that expand access to promising new medications that have not yet been approved or licensed by the agency. This accelerates drug approval by 2-3 years.
- March 31: President Ronald Reagan and French Prime Minister Jacques Chirac end an international scientific dispute when they announce that researchers from the two countries will share credit for discovery of the AIDS virus. The countries agree that patent rights to a blood test that emerged from that discovery will also be shared, with most of the royalties donated to a new foundation for AIDS research and education.
- April 7: FDA declares HIV prevention as a new indication for male condoms.
- April 19: Princess Diana makes international headlines when she is photographed shaking the hand of an HIV-positive patient in a London hospital. She goes on to become a passionate advocate for people living with HIV and to speak forcefully against HIV/AIDS-related stigma and discrimination.
- April 29: FDA approves the Western blot blood test kit, a more specific test for HIV antibodies.
- May 15: The U.S. Public Health Service adds HIV as a “dangerous contagious disease” to its immigration exclusion list and mandates testing for all visa applicants. The HIV ban will not be lifted until January 4, 2010.
- May 31: President Reagan makes his first public speech about AIDS and establishes a Presidential Commission on HIV.
- August 5: A federal judge orders Florida's DeSoto County School Board to enroll HIV-positive brothers, Ricky, Robert, and Randy Ray. The board had refused to allow the three boys, who are hemophiliacs, to attend. After the ruling, outraged town residents refuse to allow their children to attend school, and someone sets fire to the Ray house on August 28, destroying it.
- August 14: CDC issues Perspectives in Disease Prevention and Health Promotion: Public Health Service Guidelines for Counseling and Antibody Testing to Prevent HIV Infection and AIDS.
- August 18: FDA sanctions the first human testing of a candidate vaccine against HIV.
- September 30: CDC launches the first AIDS-related public service announcements, America Responds to AIDS, to kick off the newly designated AIDS Awareness Month in October.
- October 11: The AIDS Memorial Quilt goes on display for the first time on the National Mall in Washington, DC. The display features 1,920 4x8 panels and draws half a million visitors.
- October 14: In a 94-2 vote, the U.S. Senate adopts the Helms Amendment, which requires federally financed educational materials about AIDS to stress sexual abstinence and forbids any material that “promotes” homosexuality or drug use.
- October 22: AIDS becomes the first disease ever debated on the floor of the United Nations (UN) General Assembly. The General Assembly resolves to mobilize the entire UN system in the worldwide struggle against AIDS and designates the WHO to lead the effort.
- In November, journalist Randy Shilts' book about the early years of the HIV/AIDS epidemic, And the Band Played On: Politics, People and the AIDS Epidemic, is published.
- Also in November, Debra Fraser-Howze, director of teenage services at the Urban League of New York, founds the National Black Leadership Commission on AIDS. The organization works to educate, mobilize, and empower black leaders to meet the challenge of fighting HIV/AIDS and other health disparities in their local communities
- November 13: The American Medical Association declares that doctors have an ethical obligation to care for people with AIDS, as well as for those who have been infected with the virus but show no symptoms.
1988
- March 3: Ryan White, an HIV-positive teenager who has become a national spokesperson for AIDS education, testifies before the President's Commission on AIDS.
- In April, the first comprehensive needle-exchange program in North America is established in Tacoma, Washington. San Francisco then establishes what becomes the largest needleexchange program in the nation.
- May 26: The U.S. Surgeon General, C. Everett Koop, launches the U.S.'s first coordinated HIV/AIDS education campaign by mailing 107 million copies of a booklet, Understanding AIDS [PDF, 1.1 MB], to all American households. It is the largest public health mailing in history.
- July 23: FDA announces that it will allow the importation of small quantities of unapproved drugs for persons with life-threatening illnesses, including HIV/AIDS.
- October 11: ACT UP protests at FDA headquarters over the slow pace of the federal drug-approval process. Eight days later, FDA announces new regulations to speed up drug approvals.
- October 18: The Abandoned Infants Assistance (AIA) Act [PDF, 674 KB] becomes law; it addresses the issue of so-called “boarder babies.” These infants, many of whom have been perinatally exposed to drugs or HIV, have been left at hospitals indefinitely by their parents. The AIA funds demonstration projects to support moving these children into safe living arrangements.
- November 4: The Health Omnibus Programs Extension (HOPE) Act authorizes the use of federal funds for AIDS prevention, education, and testing. It is the first comprehensive federal AIDS bill, and it also establishes the National Commission on AIDS and the Office of AIDS Research at NIH.
- November 28: Elizabeth Glaser, an HIV-positive mother of two HIV-positive children, and two of her friends form the Pediatric AIDS Foundation (later renamed the Elizabeth Glaser Pediatric AIDS Foundation) to advocate for research into the care and treatment needs of children living with HIV/ AIDS.
- December 1: World AIDS Day is observed for the first time. The date is designated by WHO and supported by the UN.
- December 17: Sylvester James, Jr., an openly gay, African-American entertainer who uses only his first name, and who is called “the embodiment of disco,” dies of AIDS-related illness at age 41.
- December 20: Max Robinson, the first African- American network news anchor in the U.S., and a founder of the National Association of Black Journalists,dies of AIDS-related illness at age 49.
- December 27: Gay rights activist and writer Joseph Beam dies of an AIDS-related illness at age 33. He is best known for editing In The Life, the first collection of writing by gay black men.
- HRSA awards HIV planning grants to 11 states and 10 cities in order to create a plan for HIV/AIDS systems of care, and also funds the first Pediatric AIDS Service Demonstration Grants. These grants lay the groundwork for the statewide programs that will later be funded under the Ryan White CARE Act.
1989
- March 9: Photographer Robert Mapplethorpe dies of AIDS-related illness at age 42.
- June 16: Based on recommendations from NIH, the U.S. Public Health Service issues the first guidelines for preventing Pneumocystis carinii pneumonia, an AIDS-related opportunistic infection, and a major cause of illness and death for people living with AIDS.
- June 23: CDC releases the Guidelines for Prevention of Transmission of Human Immunodeficiency Virus and Hepatitis B Virus to Health-Care and Public- Safety Workers.
- In July, Dázon Dixon Diallo founds SisterLove, Inc., the first organization in the U.S. southeastern states to focus on women living with, or at risk for, contracting HIV.
- August 18: CDC reports that the number of reported AIDS cases in the United States has reached 100,000.
- June 23: Dr. Anthony Fauci, head of NIH's National Institute of Allergy and Infectious Diseases, endorses a “parallel track” approach to clinical trials, which will give a larger number of HIV-positive people access to experimental treatments.
- September 10–17: Members of 50 churches and mosques come together for the first Harlem Week of Prayer for the Healing of AIDS. The event is the brainchild of the Reverend Dr. Pernessa Seele, an African-American immunologist and minister, who goes on to form The Balm in Gilead, a nonprofit organization that works with black faith communities to improve health.
- September 18: The National Commission on AIDS meets for the first time.
- December 1: African-American choreographer and activist Alvin Ailey dies at age 58 of an AIDS-related illness. In 2014, President Barack Obama chooses Ailey to receive a posthumous Presidential Medal of Freedom—the nation's highest civilian honor.
- HRSA grants $20 million for HIV care and treatment through the Home-Based and Community-Based Care State grant program. For many states, this is their first involvement in HIV care and treatment.
- A CDC/HRSA initiative provides $11 million to fund seven community health centers to provide HIV counseling and testing services. This is a precursor to what will be part of the Ryan White CARE Act.
1990
>
- January 18: CDC reports the possible transmission of HIV to a patient through a dental procedure performed by an HIV-positive dentist. This episode provokes much public debate about the safety of common dental and medical procedures.
- January 26: The U.S. Public Health Service issues a statement on managing occupational exposure to HIV, including considerations regarding postexposure use of the antiretroviral drug, AZT.
- February 16: Pop artist and AIDS activist Keith Haring dies of AIDS-related illness at age 31.
- April 8: Ryan White, the Indiana teen who became an international spokesperson against HIV/AIDS stigma and discrimination, dies of AIDS-related illness at the age of 18.
- May 21: ACT UP protests at the National Institutes of Health. The group demands more HIV treatments and the expansion of clinical trials to include more women and people of color.
- June 20–24: The 6th International AIDS Conference meets in San Francisco. To protest U.S. immigration policy that bars people with HIV from entering the country, domestic and international nongovernmental groups boycott the conference.
- July 26: The U.S. Congress enacts the Americans with Disabilities Act [PDF, 7.9 MB]. The Act prohibits discrimination against individuals with disabilities, including people living with HIV/AIDS.
- August 18: The U.S. Congress enacts the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act of 1990 [PDF, 2.41 MB], which provides $220.5 million in federal funds for HIV communitybased care and treatment services in its first year. HRSA is given responsibility for managing the program, which is the nation's largest HIV-specific federal grant program.
- October 26: FDA approves use of zidovudine (AZT ) for pediatric AIDS.
- November 28: The U.S. Congress enacts legislation that includes the AIDS Housing Opportunity Act, which creates the Housing Opportunities for People with AIDS (HOPWA) program the following year. Administered by the U.S. Department of Housing and Urban Development (HUD), HOPWA grants provide housing assistance to people living with AIDS.
- December 17: In response to the critical, unmet need for HIV prevention and care among Latinos, a group of community leaders forms the Latino Commission on AIDS.
1991
- April–May: The Visual AIDS Artists Caucus launches the Red Ribbon Project to create a visual symbol to demonstrate compassion for people living with AIDS and their caregivers. The red ribbon becomes the international symbol of AIDS awareness.
- July 21: CDC recommends restrictions on the practice of HIV-positive healthcare workers. Congress goes on to enact a law requiring states to adopt the CDC restrictions or to develop and adopt their own.
- August 14: The U.S. Congress passes the Terry Beirn Community-Based Clinical Trials Program Act [PDF, 56 KB] to establish a network of community-based clinical trials for HIV treatment. Beirn, an executive and lobbyist at amfAR, played key roles in the passage of the HOPE Act and the Ryan White CARE Act. He died of AIDS-related illness on July 16, 1990, age 39.
- November 7: American basketball star Earvin “Magic” Johnson announces that he is HIV-positive.
- November 24: Freddie Mercury, lead singer/ songwriter of the rock band Queen, dies of AIDSrelated illness at age 45.
- NMAC, in cooperation with the National Association of People With AIDS (NAPWA) and the National AIDS Interfaith Network, holds the first annual National Skills Building Conference, which will later become the United States Conference on AIDS.
1992
- In this year, AIDS becomes the number one cause of death for U.S. men ages 25 to 44.
- February 4: The International Olympic Committee rules that athletes with HIV are eligible to compete in the games without restrictions.
- April 8: Arthur Ashe, the former United States Open and Wimbledon tennis champion and an African-American pioneer in sports and social issues, announces that he has AIDS. Ashe, who underwent heart-bypass surgeries in 1979 and 1983, believes he contracted HIV via blood transfusions. He dies of AIDS-related illness on February 3, 1993.
- May 11: The U.S. District Court in Manhattan declares that the Helms Amendment (1987) which requires federally financed educational materials about AIDS to stress sexual abstinence and forbids any material that “promotes” homosexuality or drug use, is unconstitutionally vague.
- May 27: FDA licenses a rapid HIV diagnostic test kit which gives results from a blood test in 10 minutes.
- July 19–24:nt.) The 8th International AIDS Conference is held in Amsterdam. The event was originally scheduled for Boston, but the venue is moved due to U.S. immigration restrictions on people living with HIV/AIDS.
- December 1: CDC launches the Business Responds to AIDS program to help large and small businesses meet the challenges of HIV/AIDS in the workplace and the community. (CDC will start the Labor Responds to AIDS program in 1995.)
1993
- President Clinton establishes the White House Office of National AIDS Policy (ONAP).
- The National Association of People With AIDS (NAPWA) convenes the first annual “AIDS Watch.” Hundreds of community members from across the U.S. come to Washington, DC, to lobby Congress for increased funding.
- January 6: World-renowned ballet dancer Rudolf Nureyev dies of AIDS-related illness at age 54.
- April 13: Angels in America, Tony Kushner's multiact play about AIDS, wins the 1993 Pulitzer Prize for drama.
- May 7: FDA approves the female condom.
- In June, the U.S. Congress enacts the NIH Revitalization Act, giving the Office of AIDS Research primary oversight of all NIH AIDS research. The Act requires NIH and other research agencies to expand involvement of women and minorities in all research.
- The same act codifies the U.S. HIV immigration exclusion policy into law; President Clinton signs it on June 10.
- In August, the Women's Interagency HIV Study and HIV Epidemiology Study begin. Both are major U.S. federally funded research studies on women and HIV/ AIDS.
- December 18: CDC expands the case definition of AIDS, declaring those with CD4 counts below 200 to have AIDS.
- In that same report, CDC adds three new conditions— pulmonary tuberculosis, recurrent pneumonia, and invasive cervical cancer—to the list of clinical indicators of AIDS. These new conditions mean that more women and people who inject drugs will be diagnosed with AIDS.
- December 22: The film Philadelphia, starring Tom Hanks as a lawyer fired from his job because he has AIDS, opens in theaters. Other earlier films, including the documentary No Sad Songs (1985), Buddies (1985), An Early Frost (1985), and Longtime Companion (1989), have addressed AIDS, but Philadelphia is the first major Hollywood film on the topic. Hanks will win his first Academy Award for Best Actor for his role.
1994
- In this year, AIDS becomes the leading cause of death for all Americans ages 25 to 44.
- February 17: Randy Shilts, a U.S. journalist who covered the AIDS epidemic and who authored And the Band Played On: Politics, People and the AIDS Epidemic, dies of AIDS-related illness at age 42.
- May 20: CDC publishes Guidelines for Preventing Transmission of Human Immunodeficiency Virus Through Transplantation of Human Tissue and Organs.
- August 5: The U.S. Public Health Service recommends that pregnant women be given the antiretroviral drug AZT to reduce the risk of perinatal transmission of HIV.
- November 11: Pedro Zamora, a member of the cast of MTV's popular television show, “The Real World,” dies of AIDS-related illness at age 22.
- December 23: FDA approves an oral HIV test, the first non-blood-based antibody test for HIV.
- HHS issues guidelines requiring applicants for NIH grants to address “the appropriate inclusion of women and minorities in clinical research.”
1995
- February 23: Olympic gold medal diver Greg Louganis discloses that he has AIDS.
- March 26: Eric Lynn Wright, a.k.a. rapper Eazy-E, dies from an AIDS-related illness, one month after being diagnosed.
- In June, FDA approves the first protease inhibitor. This ushers in a new era of highly active antiretroviral therapy (HAART ).
- June 14: President Clinton issues an Executive Order [PDF, 149 KB] establishing his Presidential Advisory Council on HIV/AIDS. The Council meets for the first time on July 28.
- June 27: The National Association of People With AIDS launches the first National HIV Testing Day.
- July 14: CDC issues the first guidelines to help healthcare providers prevent opportunistic infections in people infected with HIV.
- September 22: CDC reviews Syringe Exchange Programs -- United States, 1994-1995. The National Academy of Sciences concludes that syringe exchange programs should be regarded as an effective component of a comprehensive strategy to prevent infectious disease.
- By October 31, 500,000 cases of AIDS have been reported in the U.S.
1996
In this year, the number of new AIDS cases diagnosed in the U.S. declines for the first time since the beginning of the epidemic. The International AIDS Vaccine Initiative (IAVI) forms to speed the search for an effective HIV vaccine.
- January 1: UNAIDS (the Joint United Nations Programme on HIV/AIDS) begins operations. It is established to advocate for global action on the epidemic and to coordinate HIV/AIDS efforts acros the UN system. FDA approves:
- the first HIV home testing and collection kit (May 14)
- a viral load test, which measures the level of HIV in the blood (June 3)
- the first non-nucleoside reverse tranblockedas inhibitor (NNRTI) drug, nevirapine (June 21)
- July 7–12: In Vancouver, the 11th International AIDS Conference highlights the effectiveness of highly active antiretroviral therapy (HAART ), creating a period of optimism.
- In October, the AIDS Memorial Quilt is displayed in its entirety for the last time. It covers the entire National Mall in Washington, DC.
- December 30: TIME Magazine names HIV/AIDS researcher Dr. David Ho as its “Man of the Year” for his work on highly active antiretroviral therapy. Ho advocates for a new strategy of treating HIV – “hit early, hit hard,” in which patients are placed on new, more aggressive treatment regimens earlier in the course of their infection in hopes of keeping them healthier longer.
1997
- In this year, highly active antiretroviral therapy (HAART ) becomes the new standard of HIV care.
- CDC reports the first substantial decline in AIDS deaths in the United States. Due largely to the use of HAART, AIDS-related deaths in the U.S. decline by 47% compared with the previous year.
- May 18: President Clinton announces that the goal of finding an effective vaccine for HIV in 10 years will be a top national priority, and calls for the creation of an AIDS vaccine research center at NIH. (He dedicates the Dale and Betty Bumpers Vaccine Research Center on June 9, 1999.)
- September 26: FDA approves Combivir®, a combination of two antiretroviral drugs in one tablet, which makes it easier for people living with HIV to take their medications.
- November 21: The U.S. Congress enacts the Food and Drug Administration Modernization Act (FDAMA) of 1997, codifying an accelerated drugapproval process and allowing dissemination of information about off-label uses of drugs.
- UNAIDS estimates that 30 million adults and children worldwide have HIV, and that, each day, 16,000 people are newly infected with the virus.
- As a greater number of people begin taking protease inhibitors, resistance to the drugs becomes more common, and drug resistance emerges as an area of grave concern within the AIDS community.
1998
- CDC reports that African Americans account for 49% of U.S. AIDS-related deaths. AIDS-related mortality for African Americans is almost 10 times that of Whites and three times that of Hispanics.
- In March, African-American leaders, including members of the Congressional Black Caucus (CBC), are briefed on the highly disproportionate impact of HIV and AIDS in their communities. They develop a “Call to Action,” requesting that the President and Surgeon General declare HIV/AIDS a “State of Emergency” in the community.
- In October, President Clinton declares AIDS to be a “severe and ongoing health crisis” in African- American and Hispanic communities in the United States. He announces a special package of initiatives aimed at reducing the impact of HIV/AIDS on racial and ethnic minorities.
- With the leadership of the CBC, Congress funds the Minority AIDS Initiative [PDF, 126 KB]. An unprecedented $156 million is invested to improve the nation's effectiveness in preventing and treating HIV/AIDS in African-American, Hispanic, and other minority communities.
- April 20: HHS Secretary Donna Shalala determines that needle-exchange programs (NEPs) are effective and do not encourage the use of illegal drugs, but the Clinton Administration does not lift the ban on use of federal funds for NEPs.
- April 24: CDC issues the first national treatment guidelines for the use of antiretroviral therapy [PDF, 2.86 MB] in adults and adolescents with HIV.
- In June, UNAIDS reports [PDF, 2.34 MB] that the number of women living with HIV/AIDS in sub- Saharan Africa now exceeds that of men.
- June 25: The U.S. Supreme Court rules that the Americans with Disabilities Act covers those in earlier stages of HIV disease, not just those who have developed AIDS.
- November 12: The U.S. Congress enacts the Ricky Ray Hemophilia Relief Fund Act, [PDF, 184 KB] honoring the Florida teenager who was infected with HIV through contaminated blood products. The Act authorizes payments to individuals with hemophilia and other blood-clotting disorders who were infected with HIV by unscreened blood-clotting agents between 1982 and 1987. Ricky Ray died of AIDSrelated illness on December 13, 1992 at age 15, and Robert Ray died on October 20, 2000 at age 22.
1999
- The Congressional Hispanic Caucus, with the Congressional Hispanic Caucus Institute, convenes Congressional hearings on the impact of HIV/AIDS on the Latino community.
- WHO announces that HIV/AIDS has become the fourth biggest killer worldwide and the number one killer in Africa. The organization estimates that 33 million people are living with HIV worldwide, and that 14 million have died of AIDS.
- In March, VaxGen, a San Francisco-based biotechnology company, begins conducting the first human vaccine trials in a developing country ( Thailand).
- In May, activist Phill Wilson founds the Black AIDS Institute. The Institute's mission is “to stop the AIDS pandemic in Black communities by engaging and mobilizing Black institutions and individuals in efforts to confront HIV.” Its motto: “Our People, Our Problem, Our Solution.”
- July 19: President Clinton announces the formation of the “Leadership and Investment in Fighting an Epidemic” (LIFE) Initiative [PDF, 88 KB], which will provide funding to address the global HIV epidemic.
- December 10: CDC releases a new HIV case definition to help state health departments expand their HIV surveillance efforts and more accurately track the changing course of the epidemic.
2000
- January 10: The UN Security Council meets to discuss the impact of AIDS on peace and security in Africa. This marks the first time that the Council discusses a health issue as a threat to peace and security.
- January 27: In his State of the Union address, President Clinton announces the launch of the Millennium Vaccine Initiative to create incentives for developing and distributing vaccines against HIV, TB, and malaria.
- April 30: The Clinton Administration declares that HIV/AIDS is a threat to U.S. national security.
- May 10: President Clinton issues an Executive Order to assist developing countries in importing and producing generic HIV treatments.
- In July, UNAIDS, WHO, and other global health groups announce a joint initiative with five major pharmaceutical manufacturers to negotiate reduced prices for HIV/AIDS drugs in developing countries.
- August 19: The U.S. Congress enacts the Global AIDS and Tuberculosis Relief Act of 2000. [PDF, 2.1 MB]
- In September, as part of its Millennium Declaration, the UN adopts the Millennium Development Goals, which include a specific goal of reversing the spread of HIV/AIDS, malaria, and TB.
2001
- February 7 marks the first annual National Black HIV/AIDS Awareness Day in the U.S.
- April 23: General Colin Powell, the newly appointed U.S. Secretary of State, reaffirms the U.S. statement that HIV/AIDS is a national security threat.
- May 18 is the first annual observance of HIV Vaccine Awareness Day.
- June 25-27: The UN General Assembly holds its first Special Session on AIDS (UNGASS) and passes the UNGASS Declaration of Commitment and the ILO (International Labor Organization) Code of Practice on HIV/AIDS in the Workplace [PDF, 127 KB]. The meeting also calls for the creation of an international “global fund” to support efforts by countries and organizations to combat the spread of HIV through prevention, care, and treatment, including the purchase of HIV medications.
- November 14: The World Trade Organization announces the Doha Declaration, which affirms the rights of developing countries to buy or
- After generic drug manufacturers offer to produce discounted, generic forms of HIV/AIDS drugs for developing countries, several major pharmaceutical manufacturers agree to offer further reduced drug prices to those countries. 2001 (cont.) manufacture generic medications to meet public health crises such as HIV/AIDS.
- HRSA begins focusing on individuals with HIV disease who know their status and are not receiving HIV-related services. HRSA instructs its grantees to address this population's “unmet need” for services.
- CDC announces a new HIV Prevention Strategic Plan to cut annual HIV infections in the U.S. by half within five years.
2002
- January 22: The Global Fund to Fight AIDS, Tuberculosis and Malaria, a partnership between governments, civil society organizations, the private sector, and affected communities, is established.
- April 22-24: The Global Fund approves its first round of grants to governments and private-sector organizations in the developing world. The grants total $600 million for two-year projects.
- June 25: The United States announces a framework that will allow poor countries unable to produce pharmaceuticals to gain greater access to drugs needed to combat HIV/AIDS, malaria, and other public health crises.
- In July, UNAIDS reports that HIV/AIDS is now by far the leading cause of death in sub-Saharan Africa, and the fourth biggest global killer. Average life expectancy in sub-Saharan Africa falls from 62 years to 47 years as a result of AIDS.
- July 7-12: The 14th International AIDS Conference is held in Barcelona, Spain. Dozens of countries report they are experiencing serious HIV/AIDS epidemics, and many more are on the brink.
- In September, the U.S. National Intelligence Council releases Next Wave of the Epidemic [PDF, 3.34 MB], a report focusing on HIV in India, China, Russia, Nigeria, and Ethiopia.
- November 7: FDA approves the first rapid HIV diagnostic test kit for use in the United States that provides results with 99.6% accuracy in as little as 20 minutes. Unlike other antibody tests for HIV, this blood test can be stored at room temperature, requires no specialized equipment, and may be used outside of traditional laboratory or clinical settings, allowing more widespread use of HIV testing.
- Worldwide, 10 million young people, aged 15-24, and almost 3 million children under 15 are living with HIV. During this year, approximately 3.5 million new infections will occur in sub-Saharan Africa, and the epidemic will claim the lives of an estimated 2.4 million Africans.
2003
- CDC calculates that 27,000 of the estimated 40,000 new infections that occur each year in the U.S. result from transmission by individuals who do not know they are infected.
- January 28: President George W. Bush announces the creation of the United States President's Emergency Plan For AIDS Relief (PEPFAR) in his State of the Union address. PEPFAR is a $15 billion, 5-year plan to combat AIDS, primarily in countries with a high burden of infections.
- February 23: VaxGen, a San Francisco-based biotechnology company, announces that its AIDSVAX vaccine trial failed to reduce overall HIV infection rates among those who were vaccinated.
- March 31: The Bill and Melinda Gates Foundation awards a $60 million grant to the International Partnership for Microbicides to support research and development of microbicides to prevent transmission of HIV.
- April 18: CDC announces Advancing HIV Prevention: New Strategies for a Changing Epidemic, a new prevention initiative that aims to reduce barriers to early diagnosis and increase access to, and utilization of, quality medical care, treatment, and ongoing prevention services for those living with HIV.
- May 6: The “Group of Eight” (G8) Summit includes a special focus on HIV/AIDS and announcements of new commitments [PDF, 854 KB] to the Global Fund to Fight AIDS, Tuberculosis and Malaria. G8 members make up most of the world's largest economies and include: Canada, France, Germany, Italy, Japan, Russia, the United Kingdom, and the United States.
- October 6: Randall Tobias is sworn in as the first Ambassador at Large and U.S. Global AIDS Coordinator to oversee PEPFAR.
- October 15 marks the first annual National Latino AIDS Awareness Day in the U.S.
- October 23: The William J. Clinton Foundation secures price reductions for HIV/AIDS drugs from generic manufacturers, to benefit developing nations.
- December 1: WHO announces the “3 by 5” initiative, to bring treatment to 3 million people by 2005.
2004
- In January, the U.S. Congress authorizes the first $350 million for the United States President's Emergency Program for AIDS Relief (PEPFAR).
- In February, UNAIDS launches The Global Coalition on Women and AIDS to raise the visibility of the epidemic's impact on women and girls around the world.
- March 26: FDA approves the use of oral fluid samples with a rapid HIV diagnostic test kit that provides the result in approximately 20 minutes.
- May 17: FDA issues a guidance document for expedited approval of low cost, safe, and effective co-packaged and fixed-dose combination HIV therapies so that high-quality drugs can be made available in Africa and developing countries around the world under PEPFAR.
- June 10: Leaders of the “Group of Eight” (G8) Summit (Canada, France, Germany, Italy, Japan, Russia, the United Kingdom, and the United States) call for the creation of a “Global HIV Vaccine Enterprise,” a consortium of government and private-sector groups designed to coordinate and accelerate research efforts to find an effective HIV vaccine.
2005
- January 6: Former South African president Nelson Mandela announces that his son, Makgatho Mandela, has died of AIDS-related illness at age 54. Mandela urges South Africans to treat AIDS as an “ordinary disease,” rather than a “curse.” He also asks families to speak openly about the toll of the disease, in order to break down the taboos associated with HIV/AIDS.
- January 26–30: During its annual meeting, the World Economic Forum approves a set of new priorities, including one with a focus on addressing HIV/AIDS in Africa and other hard-hit regions.
- January 26: WHO, UNAIDS, the U.S. Government, and the Global Fund to Fight AIDS, Tuberculosis and Malaria announce results of joint efforts to increase the availability of antiretroviral drugs in developing countries. An estimated 700,000 people have been reached by the end of 2004.
- April 3: Biologists announce that they have discovered that the plagues of the Middle Ages made around 10% of Europeans—particularly those in Scandinavia and Russia—resistant to HIV.
- May 19 is the first annual National Asian and Pacific Islander HIV/AIDS Awareness Day in the U.S.
2006
- March 10 is the first annual National Women and Girls HIV/AIDS Awareness Day in the U.S.
- March 20 is the first annual observance of National Native HIV/AIDS Awareness Day in the U.S.
- May 2–6: NIH's Office of AIDS Research sponsors Embracing Our Traditions, Values, and Teachings: Native Peoples of North America HIV/AIDS Conference, in Anchorage, Alaska. The conference involves nearly 1,000 participants from the American Indian, Alaska Native, Native Hawaiian, First Nations, and U.S. Territorial Pacific Islander communities.
- May 25: Scientists announce they have spotted the signs of an HIV-like virus in chimpanzees in southern Cameroon. The discovery bolsters the theory that the first people to contract HIV did so through contact with infected blood from wild chimps in the jungle.
- May 31: The UN convenes a follow-up meeting and issues a progress report on the implementation of the Declaration of Commitment on HIV/AIDS.
- August 11: President George W. Bush appoints Dr. Mark Dybulas the Ambassador at Large and U.S. Global AIDS Coordinator to oversee the President's Emergency Plan for AIDS Relief (PEPFAR). Dybul replaces former Ambassador Randall Tobias. He is sworn in on October 10.
- August 16: WHO reports that the number of people receiving HIV antiretroviral therapy in sub-Saharan Africa has surpassed 1 million for the first time—a 10fold increase in treatment access in the region since December 2003. The increase is a result of country spending, as well as support from PEPFAR, the Global Fund to Fight AIDS, Tuberculosis and Malaria, the World Bank, pharmaceutical companies, and other bilateral donors.
- September 22: CDC releases revised HIV testing recommendations for healthcare settings, recommending routine HIV screening for all adults, aged 13-64, and yearly screening for those at high risk.
- December 13: NIH announces the early end of two clinical trials of adult male circumcision after a review of trial data reveals that medically performed circumcision reduces a man's risk of acquiring HIV through heterosexual intercourse by up to 53%.
2007
- March 28: WHO officially recommends circumcision as a way to prevent heterosexual transmission of the AIDS virus, setting the stage for donor agencies to begin paying for the operation.
- May 9: The Clinton Foundation announces it has negotiated deep price reductions for generic versions of costly, second-line AIDS drugs needed when the original medicines fail, as well as for less toxic, easier-to-use first-line medicines combined in a pill that can be taken once a day.
- May 30: In an attempt to increase the number of people taking HIV tests, WHO and UNAIDS issue new guidance recommending “provider-initiated” HIV testing in healthcare settings.
- September 21: Trials of the most promising HIV vaccine to date [STEP (HVTN 502) and Phambili (HVTN 503)] are halted after an independent Data and Safety Monitoring Board determines that the vaccine is not protecting study subjects against HIV infection. A subsequent study in 2012 will find that the vaccine actually increased participants' risk of contracting HIV, although the reasons for this are not clear.
- In October, CDC launches Prevention IS Care (PIC), a social-marketing campaign designed for healthcare providers who deliver care to people living with HIV.
- November 13: CDC reports that four transplant recipients have contracted both HIV and hepatitis C from an organ donor—the first known cases in more than a decade of the virus being spread by organ transplants. This leads to a call for more intensive testing of donor organs, which may have been infected too recently for HIV to be detected on standard tests.
- November 20: WHO and UNAIDS announce [PDF, 1.63 MB] improved surveillance data showing global HIV prevalence has levelled off, and is lower than previously believed (33 million instead of 40 million). The data also indicate declines in the numbers of new infections and people dying from AIDS-related illnesses, due in part to HIV-prevention programs and antiretroviral therapy.
- CDC reports over 565,000 people have died of AIDS in the U.S. since 1981.
2008
- January 8: The Journal of the American Medical Association reports that the incidence of HIV infection among gay men in the U.S. is increasing, following an encouraging period of decline. Between 2001–2006, new HIV diagnoses in gay men under age 30 rose 32%. Among black and Hispanic men, the figure was 34%. Most troubling, the number of new diagnoses among the youngest men in the study (ages 13–19) doubled.
- June 23: Dr. Eric Goosby is sworn in as Ambassador at Large and U.S. Global AIDS Coordinator to oversee the President's Emergency Plan for AIDS Relief (PEPFAR). He replaces Dr. Mark Dybul.
- July 25: A large international study finds evidence that people taking HIV treatment can now expect to live into their 60s and beyond. Researchers report that a 20-year-old person living with HIV who starts treatment with a CD4 cell count above 200 cells/mm3 can expect to live to be 70.
- July 29: According to a report [PDF, 1.42 MB] released by the Black AIDS Institute, the HIV/ AIDS epidemic among African-Americans in some parts of the U.S. is as severe as in parts of Africa. The report, Left Behind - Black America: A Neglected Priority in the Global AIDS Epidemic, calls for greater government investment in HIV/AIDS prevention, testing, and treatment programs in hard-hit U.S. regions.
- July 31: President George W. Bush signs legislation reauthorizing PEPFAR for an additional five years for up to $48 billion. The bill contains a rider that lifts the blanket ban on HIV-positive travelers to the U.S., and gives HHS the authority to admit people living with HIV/AIDS on a case-by-case basis.
- August 6: CDC releases new domestic HIV incidence estimates that are substantially higher than previous estimates (56,300 new infections per year vs. 40,000). The new estimates do not represent an actual increase in the numbers of HIV infections, but reflect a more accurate way of measuring new infections. A separate analysis suggests that the annual number of new infections was never as low as 40,000 and that it has been roughly stable since the late 1990s.
- September 11: A CDC study of people newly infected with HIV in the U.S. confirms that the majority of new cases occur among gay and bisexual men and that African-Americans are most at risk. But the data show that most new infections of white gay and bisexual men occur when the men are in their 30s and 40s, while black gay and bisexual men are more likely to be infected in their teens and 20s.
- September 18 marks the first observance of National HIV/AIDS and Aging Awareness Day.
- September 27 marks the first observance of National Gay Men's HIV/AIDS Awareness Day.
- October 1: An international team of researchers announces that HIV in humans may have originated as early as the 1880s. Findings from the new study suggest that the virus most likely started circulating among humans in sub-Saharan Africa sometime between 1884 and 1924 and may have been triggered by rapid urbanization in west-central Africa.
- October 1: Project Masiluleke (“lend a helping hand”) is launched in South Africa. It is the first program to use free text messages to overcome stigma and promote HIV testing and treatment. The messages include the number for the National AIDS Helpline and prompt recipients to call back the sender. The program triples the rate of calls to the helpline and surpasses the 1 billion mark in call backs within 3 years.
- October 6: The Nobel Prize in medicine is awarded to two French virologists, Françoise Barré-Sinoussi, and Luc A. Montagnier, for their 1983 discovery of HIV, the virus that causes AIDS.
2009
- Newly elected President Barack Obama calls for the development of the first National HIV/AIDS Strategy for the United States.
- In February, the District of Columbia Health Department's HIV/AIDS, Hepatitis, STD, and TB Administration reports [PDF, 7.12 MB] that Washington, DC has a higher rate of HIV (3% prevalence) than West Africa—enough to describe it as a “severe and generalized epidemic.”
- April 7: The White House and CDC launch the Act Against AIDS campaign, a multiyear, multifaceted communication campaign designed to reduce HIV incidence in the United States. CDC also launches the Act Against AIDS Leadership Initiative (AAALI), to harness the collective strength and reach of traditional, longstanding African-American institutions to increase HIV-related awareness, knowledge, and action within Black communities across the U.S.
- May 5: President Obama launches the Global Health Initiative (GHI), a six-year, $63 billion effort to develop a comprehensive approach to addressing global health in low- and middleincome countries. The United States President's Emergency Plan for AIDS Relief (PEPFAR) will serve as a core component.
- June 8 marks the first annual recognition of Caribbean American HIV/AIDS Awareness Day.
- August 17: The Department of Veterans Affairs ( VA) moves to increase the number of veterans getting HIV tests by dropping the requirement for written consent (verbal consent is still required).
- October 30: President Obama announces that his administration will officially lift the HIV travel and immigration ban in January 2010 by removing the final regulatory barriers to entry. The lifting of the travel ban occurs in conjunction with the announcement that the XIX International AIDS Conference will return to the United States for the first time in more than 20 years.
- November 24: UNAIDS reports that there has been a significant decline (-17%) in new HIV infections in the past decade. East Asia, however, has seen a dramatic 25% increase in infections over the same period.
- December 16: The U.S. Congress enacts legislation [PDF, 1.08 MB] that modifies the ban on the use of federal funds for needle-exchange programs. When applicable, federal funds may be used for personnel, equipment, syringe disposal services, educational materials, communication, marketing, and evaluation activities. On December 16, 2011, Congress reinstates the ban.
2010
- January 4: The U.S. Government officially lifts the HIV travel and immigration ban.
- March 23: President Obama signs the Patient Protection and Affordable Care Act [PDF, 2.72 KB], which expands access to care and prevention for all Americans—but offers special protections for those living with chronic illnesses, like HIV, that make it difficult for them to access or afford healthcare.
- July 13: The Obama Administration releases the first comprehensive National HIV/AIDS Strategy for the United States.
- July 19: The results of the Centre for the AIDS Programme of Research in South Africa's (CAPRISA) 004 study of antiretroviral-based vaginal microbicides are released at the 18th International AIDS Conference in Vienna, Austria. The study shows the microbicides to be safe and effective in reducing risks of new HIV infections among women by 39%. Women who use the microbicides as directed have even higher rates of protection (54%) against HIV infection.
- September 20-22: The UN convenes a summit to accelerate progress toward the 2015 Millennium Development Goals.
- Also in September, WHO, UNAIDS, and UNICEF publish their annual Universal Access report for low- and middle-income countries. The report shows an estimated 5.25 million people were receiving antiretroviral therapy in 2009, and an estimated 1.2 million people started treatment that same year – the largest annual increase yet recorded.
- November 23: NIH announces the results of the iPrEx study, showing that a daily dose of HIV drugs reduced the risk of HIV infection among HIV-negative men who have sex with men by 44%, supporting the concept of pre-exposure prophylaxis (PrEP) in a targeted population.
2011
>
- March 23: AIDS activist and award-winning actress Elizabeth Taylor dies. One of the first celebrities to advocate on behalf of people living with HIV and AIDS, Taylor was the founding national chairman of amfAR (American Foundation for AIDS Research), a nonprofit organization that supports AIDS research, HIV prevention, treatment education, and advocates for AIDS-related public policy.
- In April, public debate begins on whether the longstanding ban on transplants of HIV-infected organs should be dropped.
- June 8: HHS Secretary Sebelius hosts “Commemorating 30 Years of Leadership in the Fight Against HIV/AIDS.” Watch the Secretary's speech.
- June 8–10: Over 3,000 people participate in the United Nation's (UN) High-Level Meeting on HIV/AIDS in New York. The session recognizes critical milestones, including three decades of the pandemic and the 10-year anniversary of the 2001 UN General Assembly Special Session on HIV/AIDS and the resulting Declaration of Commitment. At the meeting, the U.S. joins with other partners in launching a global plan to eliminate mother-tochild transmission of HIV and keep mothers alive.
- July 13 marks the one-year anniversary of the White House National HIV/AIDS Strategy. The White House release a video: “President Obama's National HIV/AIDS Strategy“ and the “National HIV/AIDS Strategy: Implementation Plan Update“ [PDF, 387 KB].
- July 13: A new CDC study (TDF2) [PDF, 130 KB] and a separate clinical trial (the Partners PrEP study) [PDF, 144 KB] provide the first evidence that a daily oral dose of antiretroviral drugs used to treat HIV infection can also prevent new infections in individuals exposed to HIV through heterosexual sex.
- AIDS Action merges with the National AIDS Fund to form AIDS United.
- July 17-20: At the International AIDS Society's Conference on HIV Pathogenesis, Treatment, and Prevention in Rome, scientists announce that two studies have confirmed that individuals taking daily antiretroviral drugs experienced infection rates more than 60% lower than those on a placebo.
- September 30: A coalition of community-based organizations joins with the International AIDS Society to kick off the first Road to AIDS 2012 Town Hall meeting in San Francisco. This is the first of 15 meetings to be held across the country, leading up to the XIX International AIDS Conference (AIDS 2012).
- November 8: Secretary of State Hillary Rodham Clinton shares the U.S. Government's bold new vision of creating an AIDS-free generation and speaks about the remarkable progress made in 30 years of fighting AIDS.
- December 1: At the ONE Campaign and (RED) event in Washington, DC, President Obama marks World AIDS Day by announcing accelerated efforts to increase the availability of treatment to people living with HIV/AIDS in the United States. He challenges the global community to deliver funds to The Global Fund to Fight AIDS, Tuberculosis and Malaria, and calls on Congress to keep its past commitments intact. He calls on all Americans to keep fighting to end the epidemic.
- December 1: Lead federal agencies release implementation plans in support of the U.S. National HIV/AIDS Strategy.
- December 23: The journal Science announces that it has chosen the HPTN 052 study as its 2011 Breakthrough of the Year.
2012
- March 13: Researchers from the University of New South Wales in Australia find that people living with HIV who are taking antiretroviral therapy have an increased risk of cardiovascular disease.
- March 27: HHS issues new HIV treatment guidelines recommending treatment for all HIVinfected adults and adolescents, regardless of CD4 count or viral load.
- June 20: The Washington, DC, Department of Health releases a study showing a drop in the overall number of new AIDS cases in the District over four years and improvements in getting infected people into care quickly. But the progress is uneven: HIV infection rate for heterosexual African-American women in the District's poorest neighborhoods nearly doubled in two years, from 6.3% to 12.1%.
- July 1: The Kaiser Family Foundation and the Washington Post release a joint survey of the American public's attitudes, awareness, and experiences related to HIV and AIDS. The survey finds that roughly a quarter of Americans do not know that HIV cannot be transmitted by sharing a drinking glass—almost exactly the same share as in 1987.
- July 3: The FDA approves the first at-home HIV test that will let users learn their HIV status right away.
- July 16: The FDA approves the use of Truvada® for pre-exposure prophylaxis (PrEP). Adults who do not have HIV, but who are at risk for infection, can now take this medication to reduce their risk of getting the virus through sexual activity.
- July 22-27: The XIX International AIDS Conference (AIDS 2012) is held in Washington, DC—the first time since 1990 that the conference has been held in the United States. Conference organizers had refused to convene the event in the U.S. until the federal government lifted the ban on HIV-positive travelers entering the country.
- During AIDS 2012, the AIDS Memorial Quilt is displayed in its entirety in Washington, DC, for the first time since 1996. Volunteers have to rotate nearly 50,000 panels to ensure that the entire work is displayed.
2013
- The U.S. President's Emergency Plan for AIDS Relief (PEPFAR) celebrates its 10th anniversary.
- March 4: NIH-funded scientists announce the first well-documented case of an HIV-infected child, designated as “the Mississippi Baby,” who appears to have been functionally cured of HIV infection (i.e., no detectable levels of virus or signs of disease, even without antiretroviral therapy).
- June 2: The New York Times runs two articles which focus on middle-aged people living with HIV: The Faces of H.I.V. in New York in 2013 and ‘People Think It's Over': Spared Death, Aging People With H.I.V. Struggle to Live.
- June 5: NMAC releases RISE Proud: Combating HIV Among Black Gay and Bisexual Men [PDF, 1.4 MB], an action plan to mitigate the impact of HIV on black gay and bisexual men.
- June 18: Secretary of State John Kerry announces that, thanks to direct PEPFAR support, more than 1 million infants have been born HIV-free since 2003.
- July 3: Researchers report that two HIV-positive patients in Boston who had bone-marrow transplants for blood cancers have apparently been virus-free for weeks since their antiretroviral drugs were stopped.
- July 13: President Obama issues an Executive Order directing federal agencies to prioritize supporting the HIV care continuum as a means of implementing the National HIV/AIDS Strategy. The HIV Care Continuum Initiative aims to accelerate efforts to improve the percentage of people living with HIV who move from testing to treatment and—ultimately—to viral suppression.
- In October, the National Latino AIDS Action Network —a diverse coalition of communitybased organizations, national organizations, state and local health departments, researchers and concerned individuals—publishes the National Latino/Hispanic HIV/AIDS Action Agenda [PDF, 4.1 MB] to raise awareness, identify priorities, and issue specific recommendations to address the impact of the epidemic in Hispanic/Latino communities.
- November 1: Dallas Buyers Club—a film about an HIV-positive man who smuggled unapproved HIV drugs from Mexico to meet the demands of people who were dying of AIDS—is released to wide critical acclaim. The film, which is based on the true story of Texas electrician Ron Woodroof, goes on to win three Academy Awards. Woodroof died of AIDS-related illness on September 12, 1992.
- November 21: President Obama signs the HIV Organ Policy Equity (HOPE) Act, which will allow people living with HIV to receive organs from other infected donors. The HOPE Act has the potential to save the lives of about 1,000 HIV-infected patients with liver and kidney failure annually.
- December 5: Nelson Mandela —South African anti-apartheid leader, political prisoner, and national President from 1994 to 1999—dies at the age of 95. After his son, Makgatho, died of AIDS-related causes in 2005, Mandela spent the remainder of his postpresidential career working to address the AIDS epidemic in South Africa, which is home to the largest number of people living with HIV (~6.8 million) in the world.
- At the end of 2012, UNAIDS estimates that, worldwide, 2.3 million people were newly infected with HIV during the year, and 1.6 million people died of AIDS. Approximately 35.3 million people around the world are now living with HIV, including more than 1.2 million Americans [PDF, 477 KB].
- UNAIDS also announces that new HIV infections have dropped more than 50% in 25 low- and middleincome countries, and the number of people getting antiretroviral treatment has increased 63% in the past two years.
2014
- January 1: Major provisions of the Affordable Care Act designed to protect consumers go into effect. Insurers are now barred from discriminating against customers with pre-existing conditions, and they can no longer impose annual limits on coverage—both key advances for people living with HIV/AIDS.
- January 2: News sources report that the two Boston patients believed to have been cured of HIV after undergoing treatment for cancer have relapsed.
- In March, the UN Commission on the Status of Women releases a report [PDF, 563 KB] on the challenges and achievements of implementing the Millennium Development Goals (MDGs) for women and girls. The Commission concludes that progress on MDG6 (Combating HIV/AIDS, Malaria, and Other Diseases) has been limited, given that the number of women living with HIV globally continues to increase. The report notes several key challenges: adolescent/young women's particular vulnerability to HIV; the need to increase access to healthcare services; and the challenges of structural gender inequalities, stigma, discrimination, and violence.
- March 4: European researchers announce the results of the first phase of the PARTNER Study, an observational study focusing on the risk of sexual HIV transmission when an HIV-positive person is on treatment. The study found that no HIV-positive partner who was undergoing antiretroviral therapy and had an undetectable viral load had transmitted HIV.
- March 24: Douglas Brooks is appointed as the new Director of the White House Office of National AIDS Policy (ONAP). He is the first African-American and the first HIV-positive person to hold the position.
- April 4: Dr. Deborah Birx is sworn in as Ambassador at Large and U.S. Global AIDS Coordinator to oversee the President's Emergency Plan for AIDS Relief (PEPFAR). She replaces Dr. Eric Goosby.
- July 10: NIH announces that the “Mississippi baby” now has detectable levels of HIV after more than two years of showing no evidence of the virus.
- July 17: Malaysia Airlines' Flight MH17, en route from Amsterdam to Kuala Lumpur, is shot down over conflict-ridden Ukraine, killing all 298 people aboard—including six prominent scientists and AIDS activists on their way to the 20th International AIDS Conference (AIDS 2014) in Melbourne, Australia.
- July 20-25: AIDS 2014 draws nearly 14,000 delegates from over 200 nations. One key message of the conference is that a one-size-fits-all approach may not be suitable for all settings, [PDF, 4.6 MB] especially given the diversity of the epidemic's geographical hotspots and key populations. Interventions and policies will require target-based strategies and greater support of key populations, especially in countries where discriminatory policies and legislation are hindering prevention and treatment efforts.
- September 9: The Pew Charitable Trust reports that southern states are now the epicenter of HIV/AIDS in the U.S.
- October 9: CDC releases a new report that finds gaps in care and treatment among Latinos diagnosed with HIV.
- November 25: CDC announces that only 30% of Americans with HIV had the virus under control in 2011. Approximately two-thirds of those whose virus was out of control have been diagnosed but are no longer in care.
2015
- January 8: A review of multiple studies of South African women indicates that using Depo Provera®, an injectable contraceptive, may increase women's chances of contracting HIV by 40%.
- February 23: CDC's annual HIV Surveillance Report [PDF, 2.8 MB], indicates that HIV diagnosis rates in the U.S. remained stable between 2009-2013, but men who have sex with men, young adults, racial/ ethnic minorities, and individuals living in the South continue to bear a disproportionate burden of HIV.
- February 23: CDC announces that more than 90% of new HIV infections in the United States could be prevented by diagnosing people living with HIV and ensuring they receive prompt, ongoing care and treatment.
- February 25: Indiana state health officials announce an HIV outbreak linked to injection drug use [PDF, 59 KB] in the southeastern portion of the state. By the end of the year, Indiana will confirm 184 new cases of HIV linked to the outbreak.
- May 8:HHS announces plans to amend the federal rules covering organ transplants to allow the recovery of transplantable organs from HIVpositive donors. The new regulations will provide a framework for clinical studies on transplanting organs from HIV-positive donors to HIV-positive recipients.
- May 27: Results from the Strategic Timing of AntiRetroviral Treatment (START ) study indicate that HIV-positive individuals who start taking antiretroviral drugs before their CD4 cell counts decrease have a considerably lower risk of developing AIDS or other serious illnesses. Subsequent data releases show that early therapy for people living with HIV also prevents the onset of cancer, cardiovascular disease, and other non-AIDSrelated diseases.
- June 30: WHO certifies that Cuba is the first nation to eliminate mother-to-child transmission of both HIV and syphilis.
- July 14: UNAIDS announces that the targets for Millennium Development Goal #6 —halting and reversing the spread of HIV—have been achieved and exceeded 9 months ahead of the schedule set in 2000.
- July 20: Researchers report that antiretroviral therapy is highly effective at preventing sexual transmission of HIV from a person living with HIV to an uninfected heterosexual partner, when the HIV-positive partner is virally suppressed. The finding comes from the decade-longHPTN 052 clinical trial.
- July 30: The White House launches the National HIV/AIDS Strategy: Updated to 2020 [PDF, 2.2 MB]. The updated Strategy retains the vision and goals of the original, but reflects scientific advances, transformations in healthcare access as a result of the Affordable Care Act, and a renewed emphasis on key populations, geographic areas, and practices necessary to end the domestic HIV epidemic.
- September 26: At a UN summit on the Sustainable Development Goals, the United States announces new PEPFAR prevention and treatment targets [PDF, 640 KB] for 2016–2017. By the end of 2017, the U.S. will commit sufficient resources to support antiretroviral therapy for 12.9 million people, provide 13 million male circumcisions for HIV prevention, and reduce HIV incidence by 40% among adolescent girls and young women within the highest burdened areas of 10 sub-Saharan African countries.
- September 30: The WHO announces new treatment recommendations that call for all people living with HIV to begin antiretroviral therapy as soon after diagnosis as possible. WHO also recommends daily oral PrEPas an additional prevention choice for those at substantial risk for contracting HIV. WHO estimates the new policies could help avert more than 21 million deaths and 28 million new infections by 2030.
- October 20: Greater Than AIDS launches a new campaign, Empowered: Women, HIV and Intimate Partner Violence to bring more attention to issues of relationship violence and provide resources for women who may be at risk of, or dealing with, abuse and HIV.
- November 17: Actor Charlie Sheen announces his HIV-positive status in a nationally televised interview. Significant public conversation about HIV follows his disclosure. Other celebrities who disclose their HIVpositive status in 2015 are rapper, performance artist, and poet Mykki Blanco and former child TV star Danny Pintauro.
- November 24: UNAIDS releases its 2015 World AIDS Day report [PDF, 27 MB], which finds that 15.8 million people were accessing antiretroviral treatment as of June 2015—more than doubling the number of people who were on treatment in 2010.
- November 30: amfAR announces its plan to establish the Institute for HIV Cure Research at the University of California, San Francisco. As the cornerstone of amfAR's $100 million investment in cure research, the Institute will work to develop the scientific basis for an HIV cure by the end of 2020.
- December 1: The White House releases a Federal Action Plan [PDF, 772 KB] to accompany the updated National HIV/AIDS Strategy. The plan was developed by 10 federal agencies and the Equal Employment Opportunity Commission and contains 170 action items that the agencies will undertake to achieve the goals of the Strategy.
- December 6: CDC announces that annual HIV diagnoses in the U.S. fell by 19% from 2005 to 2014. There were steep declines among heterosexuals, people who inject drugs, and African-Americans (especially black women), but trends for gay/bisexual men varied by race/ethnicity. Diagnoses among white gay/bisexual men decreased by 18%, but they continued to rise among Latino gay/bisexual men ( 24%) and black gay/bisexual men ( 22%), although the increase for the latter leveled off since 2010.
- December 19: Partly in response to the HIV outbreak in Indiana, which is linked to injection drug use, Congress modifies restrictions that prevented states and localities from spending federal funds for needle exchange programs.
- December 21: FDA announces it will lift its 30-yearold ban on all blood donations by men who have sex with men and institute a policy that allows them to donate blood if they have not had sexual contact with another man in the previous 12 months.
2016
- January 19: CDC reports that only 1 in 5 sexually active high school students has been tested for HIV. An estimated 50% of young Americans who are living with HIV do not know they are infected.
- January 28: Researchers announce that an international study of over 1,900 patients with HIV who failed to respond to the antiretroviral drug tenofovir—a key HIV treatment medication— indicates that HIV resistance to the medication is becoming increasingly common.
- February 25: At the annual Conference on Retroviruses and Opportunistic Infections (CROI), researchers report that a man taking the HIVprevention pill Truvada® has contracted HIV—marking the first reported infection of someone regularly taking the drug.
- March 3: The White House Office of National AIDS Policy, the NIH Office of AIDS Research, and the National Institute of Mental Health cohost a meeting to address the issue of HIV stigma: Translating Research to Action: Reducing HIV Stigma to Optimize HIV Outcomes. Participants include researchers, policymakers, legal scholars, faith leaders, advocates, and people living with HIV.
- March 3: Pharmacy researchers report finding that women need daily doses of the antiviral medication Truvada® to prevent HIV infection, while men only need two doses per week due to differences in the way the drug accumulates in vaginal, cervical and rectal tissue.
- March 29: HHS releases new guidance [PDF, 960 KB] for state, local, tribal, and territorial health departments that will allow them to request permission to use federal funds to support syringeservices programs (SSPs). The funds can now be used to support a comprehensive set of services, but they cannot be used to purchase sterile needles or syringes for illegal drug injection.
- May 24:NIH and partners announce they will launch a large HIV vaccine trial in South Africa in November 2016, pending regulatory approval. This represents the first time since 2009 that the scientific community has embarked on an HIV vaccine clinical trial of this size.
- June 8-10: The UN holds its 2016 High-Level Meeting on Ending AIDS. UN member states pledge to end the AIDS epidemic by 2030, but the meeting is marked by controversy after more than 50 nations block the participation of groups representing LGBT people from the meeting. The final resolution barely mentions those most at risk for contracting HIV/ AIDS: men who have sex with men, sex workers, transgender people and people who inject drugs.
Disclaimer and Acknowledgements
The information contained in this timeline has been drawn from numerous sources, including (but not limited to) the Kaiser Family Foundation ,AIDS Action (PDF), Australia's Albion Center ( PDF), and the National Minority AIDS Council (NMAC).
We have also relied on material provided by the U.S. Centers for Disease Control and Prevention (CDC), the National Institutes of Health (NIH), the U.S. Food and Drug Administration (FDA), and the U.S. Health Resources and Services Administration (HRSA).
The timeline is presented for informational purposes only. AIDS.gov does not endorse any organization or viewpoint represented in entries drawn from non-Federal sources. Where possible, specific dates have been provided and events have been listed in chronological order. Entries without specific dates occurred in the year in which they are listed, but the order of those entries may not reflect the actual chronology of events.
Every attempt has been made to ensure that the information contained in the timeline is accurate. Please send any corrections to contact@aids.gov.
https://www.hiv.gov/sites/default/files/aidsgov-timeline.pdf
D. Making A Difference
1. Supporting Someone Living with HIV
How Can You Help Someone Who Has Been Newly Diagnosed with HIV? There are many things that you can do to help a friend or loved one who has been recently diagnosed with HIV:
- Talk. Be available to have open, honest conversations about HIV. Follow the lead of the person who is diagnosed with HIV. They may not always want to talk about it, or may not be ready. They may want to connect with you in the same ways they did before being diagnosed. Do things you did together before their diagnosis; talk about things you talked about before their diagnosis. Show them that you see them as the same person and that they are more than their diagnosis.
- Listen. Being diagnosed with HIV is life-changing news. Listen to your loved one and offer your support. Reassure them that HIV is a manageable health condition. There are medicines that can treat HIV and help them stay healthy.
- Learn. Educate yourself about HIV: what it is, how it is transmitted, how it is treated, and how people can stay healthy while living with HIV. Having a solid understanding of HIV is a big step forward in supporting your loved one. This website is a good place to begin to familiarize yourself with HIV. Have these resources available for your newly diagnosed friend if they want them. Knowledge is empowering, but keep in mind that your friend may not want the information right away.
- Encourage treatment. Some people who are recently diagnosed may find it hard to take that first step to HIV treatment. Your support and assistance may be helpful. By getting linked to HIV medical care early, starting treatment with HIV medication (called antiretroviral therapy or ART), adhering to medication, and staying in care, people with HIV can keep the virus under control, and prevent their HIV infection from progressing to AIDS. HIV treatment is recommend for all people with HIV and should be started as soon as possible after diagnosis. Encourage your friend or loved one to see a doctor and start HIV treatment as soon as possible. If they do not have an HIV care provider, you can help them find one. There are programs that can provide HIV medical care or help with paying for HIV medications. Use HIV.gov's HIV Testing Sites & Care Services Locator to find a provider.
- Support medication adherence. It is important for people living with HIV to take their HIV medication every day, exactly as prescribed. Ask your loved one what you can do to support them in establishing a medication routine and sticking to it. Also ask what other needs they might have and how you can help them stay healthy. Learn more about treatment adherence.
- Get support. Take care of yourself and get support if you need it. Turn to others for any questions, concerns, or anxieties you may have, so that the person who is diagnosed can focus on taking care of their own health.
If you are the sexual partner of someone who has been diagnosed with HIV, you should also get tested so that you know your own HIV status. If you test negative, talk to your healthcare provider about PrEP (pre-exposure prophylaxis), taking HIV medicine daily to prevent HIV infection. PrEP is recommended for people at high risk of HIV infection, including those who are in a long-term relationship with a partner who has HIV. If you test positive, get connected to HIV treatment and care as soon as possible. What If a Friend Tells You That They Have HIV? More than a million people in the United States are living with HIV, so you may know someone who has the virus. If your friend, family member, or co-worker has been HIV-positive for some time and has just told you, here's how you can be supportive:
- Acknowledge. If someone has disclosed their HIV status to you, thank them for trusting you with their private health information.
- Ask. If appropriate, ask if there's anything that you can do to help them. One reason they may have chosen to disclose their status to you is that they need an ally or advocate, or they may need help with a particular issue or challenge. Some people are public with this information; other people keep it very private. Ask whether other people know this information, and how private they are about their HIV status.
- Reassure. Let the person know, through your words or actions, that their HIV status does not change your relationship and that you will keep this information private if they want you to.
- Learn. Educate yourself about HIV. Today, lots of people living with HIV are on ART and have the virus under control. Others are at different stages of treatment and care. Don't make assumptions and look to your friend for guidance.
2. Getting Involved
How Can I Help End HIV? Want to get involved in HIV-related efforts? Here are some ideas: Reach out to a local HIV service organization. Many HIV service organizations have opportunities for people living with HIV and others to share their time and talents. Depending on the organization, volunteer opportunities may include:
- Assisting with onsite or mobile testing events by being a greeter, registrar, health educator, or HIV tester
- Providing administrative support, such as filing, data entry, or answering phones
- Helping out with special events
- Participating in fundraising or advocacy activities
- Providing language skills
- Offering professional services, such as legal assistance or medical care, if licensed
To find a local HIV service organization near you, use HIV.gov's HIV Testing Sites & Care Services Locator Engage with others. Social media tools like Facebook, Twitter, Instagram and Snapchat offer many opportunities to connect with others who are interested and involved in HIV issues. You can also share information about HIV via these channels to help others learn more. Get involved in HIV awareness days. Check out our HIV awareness days page to see how you can support national observances to raise awareness and encourage people to get tested for HIV, seek, or return to care. Learn. Stay abreast of changes in HIV prevention, care, treatment and research and learn about new tools or resources. Check out our learning opportunities page to find webinars, conferences, Twitter chats, and other events.
Share what you know. You can make a difference by learning more about HIV and sharing that knowledge with others. Talk to others about testing, how to prevent HIV, the effectiveness of treatment, and the importance of getting and staying in medical care. Use our Basics pages to find answers to questions you or others may have. You can easily share those pages on social media or via email using the buttons at the top right side of each page.
3. Standing Up To Stigma
How Can You Stand Up to HIV-Related Stigma?
HIV-related stigma and discrimination still persist in the United States and negatively affect the health and well-being of people living with HIV. You can play an important role in reducing stigma and discrimination by offering your support to people living with HIV and speaking out to correct myths and stereotypes that you hear from others in your community.
- Need inspiration? View the personal stories of people who are living healthy with HIV. Visit Positive Spin.
- Want to learn more? CDC's Let's Stop HIV Together campaign raises awareness about HIV and its impact on the lives of all Americans and fights
stigma by showing that persons with HIV are real people—mothers, fathers, friends, brothers, sisters, sons, daughters, partners, wives, husbands, and co-workers. Almost 8 in 10 HIV patients in the United States report feeling internalized HIV-related stigma, according to a CDC study. Internalized stigma is when a person living with HIV experiences negative feelings or thoughts about their HIV status. Read more about this and about how people living with HIV can reduce internalized stigma? Read about what federal agencies are doing to confront and reduce HIV-related stigma.
----------------------------------------------------------------------------------------------------------------------- [ QN.No.#1. What is HIV? a) a deadly virus that can now be treated and eradicated in the body b) a disease caused by an uncontrolled division of abnormal cells in a part of the body c) a virus that attacks cells that help the body fight infection d) a disease that affects the exocrine glands producing abnormal secretions ] [ QN.No.#2. What is AIDS? a) the late stage of HIV infection that occurs when the body's immune system is badly damaged b) a disease, even with treatment, that has an estimated 1 percent survival rate one year after diagnosis c) a chronic bacterial disease d) an abnormal buildup of cerebrospinal fluid in the ventricles of the brain because of HIV] [ QN.No.#3. In the U.S., most people with HIV do not develop AIDS because taking HIV medicine every day as prescribed stops the progression of the disease. True or False? a) True
b) False] [ QN.No.#4. HIV testing… a) is invasive and painful b) should only be conducted if you exhibit symptoms of illness c) is not necessary if you do not share needles d) is relatively simple] [ QN.No.#5. HIV can be transmitted through all of the following except: a) blood and breast milk b) semen (cum) and pre-seminal fluid c) rectal and vaginal fluids d) sweat] [ QN.No.#6. In the United States, the two most common ways of contracting HIV is through: a) having vaginal or anal sex with someone who has HIV; and sharing injection drug equipment, such as needles b) sharing injection drug equipment, such as needles; and having oral sex c) having oral sex; and receiving a blood transfusion d) receiving a blood transfusion; and having vaginal or anal sex with someone who has HIV] [ QN.No.#7. People with HIV who take HIV medicine daily as prescribed and get and keep an undetectable viral load have effectively no risk of transmitting HIV to an HIV-negative partner through sex. True or False? a) True
b) False] [ QN.No.#8. Stage 2: Clinical Latency is described as a stage that/when.. (b) a) presents with flu-like symptoms that last several weeks b) the virus multiplies, but at very low levels and can last for 10 to 15 years c) includes rapid weight loss, Pneumonia, memory loss and depression d) requires the patient staying in bed all day either watching television or resting] [ QN.No.#9. Approximately ______ million people in the U.S. are living with HIV today. About ___ percent of them (____) are unaware they are infected. a) 10.1 million, 8 percent, 1 in 15 b) 1.1 million, 15 percent, 1 in 7 c) 2.5 million, 15 percent, 1 in 14 d) 3.7 million, 10 percent, 1 in 23] [ QN.No.#10. The population most affected by HIV is/are: a) lesbian and bisexual women b) heterosexual men c) gay and bisexual men d) bisexual women ] [ QN.No.#11. _______________ account for a higher proportion of new HIV diagnoses and people living with HIV, compared to other races/ethnicities. a) Native Americans b) Asian Americans c) Blacks/African Americans d) Hispanics]
|
|