|
HIV / AIDS Course > Chapter 6 - Staying in HIV Care
|
|||||||||||||||||||||||||||||||||||||||||
Chapter 6: Staying in HIV CareA. Provider Visits and Lab Tests:1. Making Care Work for You What Are the Benefits of Staying in HIV Medical Care?
HIV treatment is a lifelong commitment to your health and well-being. People who are newly diagnosed with HIV often find it overwhelming. But HIV is a manageable disease. People living with HIV who take their HIV medications every day exactly as prescribed and achieve and maintain a suppressed viral load can live long and healthy lives and have effectively no risk of transmitting the virus to their sexual partners. See Your HIV Health Care Provider Regularly Part of keeping the virus in check and staying healthy is seeing your HIV health care provider regularly—usually a couple of times a year, depending on your health. At your HIV medical care appointments, your provider will run blood tests to monitor your HIV infection and make sure your HIV medication is working properly. He or she will also treat you for other health concerns you may have, and help connect you to resources to help you with other issues that could affect your ability to stick to your HIV treatment plan. If you don't have a provider or want to find a new one, get tips on how to locate an HIV health care provider. How Can You Make the Most of Your Medical Care? HIV care and treatment is most successful when you actively take part. That means taking your HIV medications as prescribed, keeping your medical appointments, and communicating honestly with your health care provider. However, health care providers know that taking HIV medication every day and seeing a HIV health care provider regularly can be difficult for some people. For example, some people may experience side effects from medication. Others may have trouble taking their medication on time given a busy work schedule. If you're having trouble taking your HIV medication and staying in medical care, talk to your provider right away. Together you can identify the reasons and make a plan to address them. You can find the support and assistance you need. For example, you might find it useful to join a support group with other people living with HIV. Or your HIV care team might be able to connect you to a peer mentor who has been down this road and can share lessons and perspectives that might be helpful. Many HIV care teams also offer case management services to help connect you to other supportive services that can help you overcome other obstacles to remaining in regular HIV medical care. Taking the steps that are necessary for you to get control over the virus will make it easier for you to put more time and energy toward the other parts of your life. Once you find a strategy works for you, HIV can become a routine part of your life. If unexpected things happen that make it harder to manage life with HIV again, step back and think about what has changed. Don't be too hard on yourself and give up. Get support from others and learn from their experiences. Think about some of the barriers that you have already overcome, and remind yourself of your strengths and abilities. You can make HIV care work for you. Some of the other information on this site may be useful to you in figuring this out, especially the information about HIV treatment, mental health, substance use and other topics related to living well with HIV. Content Source: HIV.gov Date last updated: September 27, 2018 2. Seeing Your Health Care ProviderManaging Your Appointments
HIV is a treatable condition. If you are diagnosed early, get on antiretroviral therapy (ART), and adhere to your medication, you can stay healthy, live a normal life span, and reduce the chances of transmitting HIV to others. Part of staying healthy is seeing your HIV care provider regularly so that he or she can track your progress and make sure your HIV treatment is working for you. Your HIV care provider might be a doctor, nurse practitioner, or physician assistant. Some people living with HIV go to an HIV clinic; others see an HIV specialist at a community health center, Veterans Affairs clinic, or other health clinic; and some people see their provider in a private practice. Current guidelines recommend that most people living with HIV see their provider for lab tests every 3 to 4 months. Some people may see their provider more frequently, especially during the first two years of treatment or if their HIV viral load is not suppressed (i.e. very low or undetectable). Current guidelines say that people who take their medication every day and have had a suppressed viral load at every test for more than 2 years only need to have their lab tests done two times a year. In addition to seeing your HIV care provider, you may need to see other health care practitioners, including dentists, nurses, case managers, social workers, psychiatrists/psychologists, pharmacists and medical specialists. This may mean juggling multiple appointments, but it is all part of staying healthy. You can help make this easier by preparing a plan for yourself. Before Your Visit For many people living with HIV, appointments with their HIV care provider become a routine part of their life. These tips may help you better prepare for your visits to your HIV care provider and get more out of them:
During Your Visit
Asking Questions and Solving Problems It's important for you to be an active participant in your own health care and it's your right to ask questions. You may need to direct your questions to different people, depending on what you need/want to know:
Dental Appointments Dental visits are an extremely important part of your care when living with HIV. Many signs of HIV infection can begin in the mouth and throat, and people with HIV are more likely to develop some serious dental problems. For these reasons, it is important to see a dentist regularly. Tips for your dental visit:
Content Source: HIV.gov Date last updated: May 15, 2017 3. Lab Tests and ResultsLab Tests and Why They Are Important As part of your HIV care, your provider will order several laboratory tests. The results of these lab tests, along with your physical exam and other information you provide, will help you and your provider work together to develop the best plan to manage your HIV care so that you can get the virus under control, protect your health, and reduce the chance that you will pass the virus to others. Your healthcare provider will repeat some of these tests as part of your ongoing HIV care to continue to assess your health and how well your HIV treatment is working.
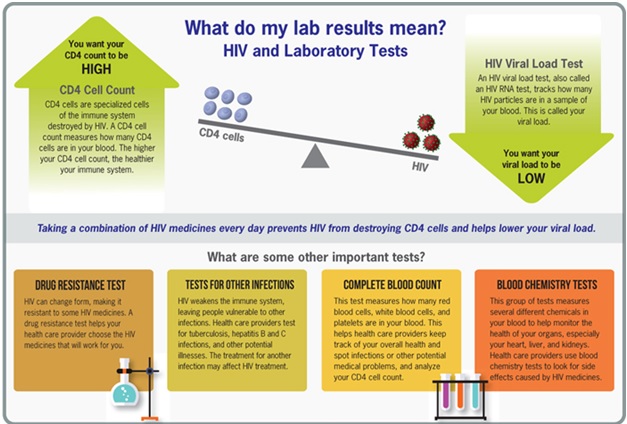 The lab tests may include:
Content Source:HIV.gov Date last updated: February 14, 2017 4.Returning to CareWhat Should You Do If You've Stopped Going to HIV Care?
If you've stopped seeing your health care provider regularly for HIV care or have stopped taking your medication, it's important to return to care, even if you have to start seeing a new provider. HIV is a serious health condition. If you stop taking your HIV medication or haven't seen a health care provider recently for a test to know if your medication is working, you are giving HIV the chance to multiply quickly. This could weaken your immune system, and you could become very sick. You could also develop resistance your HIV medications, and they will no longer be as effective. Some people living with HIV who stop seeing their health care provider worry about going back and how their provider will react. But providers are usually concerned when their patients stop coming to appointments and are happy to see them return to care. Talk openly and honestly with your provider. Discuss the reasons why you haven't kept up with your appointments and/or have stopped taking your HIV medications so that he or she can help you find ways to address those reasons in the future. And if you don't like your health care provider, find a new one. Your new provider can help you ask for your health records to be transferred over from your previous provider. Remember: Being in care and taking your HIV medication is the key to staying healthy. You can manage your HIV and live a long, healthy life with regular medical care and HIV treatment. Help Is Available Reach out to a local HIV/AIDS service organization. They have lots of experience helping people who have left HIV care and want to return. Many organizations have peer navigators. These are individuals from the community who are trained to guide you through the medical and social services you may need and provide support to help you stick to your HIV treatment plan. Many are living with HIV themselves and have learned a lot about how to make it easier to take medication and remain in care. They can relate to your experience and work with you to develop solutions to many problems you may encounter. Many organizations also have case managers or benefits counselors who can help you determine what programs and services you may qualify for—as well as help you find support groups. To find a local HIV/AIDS service organization near you, use the HIV Testing and Care Services Locator. Reasons People Stop Going to HIV Care There are many reasons why some people stop taking their HIV medication and stop seeing their health care provider regularly. These include medication side effects that are difficult to manage, changes in health care coverage, moving to different city or state, or other issues such as substance abuse or mental health disorders. Read about these challenges and how you might overcome them on our page, Tips for Taking Your HIV Medications Every Day. Need inspiration to return to care? View the personal stories of people living with HIV who are living healthy with HIV. Visit PositiveSpin.HIV.gov. Content Source: HIV.gov Date last updated: May 15, 2017 B. HIV Treatment1. HIV Treatment OverviewWhat Is HIV Treatment?
HIV treatment involves taking medicines that slow the progression of the virus in your body. HIV is a type of virus called a retrovirus, and the combination of drugs used to treat it is called antiretroviral therapy (ART). ART is recommended for all people living with HIV, regardless of how long they've had the virus or how healthy they are. ART must be taken every day, exactly as your health care provider prescribes. Why Is HIV Treatment Important? Getting and staying on HIV treatment because it reduces the amount of HIV in your blood (also called the viral load) to a very low level. This keeps you healthy and prevents illness. There is also a major prevention benefit. People living with HIV who take HIV medication daily as prescribed and get and keep an undetectable viral load have effectively no risk of sexually transmitting HIV to their HIV-negative partners. This is called treatment as prevention. If left untreated, HIV attacks your immune system and can allow different types of life-threatening infections and cancers to develop. If your CD4 cell count falls below a certain level, you are at risk of getting an opportunistic infection. These are infections that don't normally affect people with healthy immune systems but that can infect people with immune systems weakened by HIV infection. Your health care provider may prescribe medicines to prevent certain infections. HIV treatment is most likely to be successful when you know what to expect and are committed to taking your medicines exactly as prescribed. Working with your health care provider to develop a treatment plan will help you learn more about HIV and manage it effectively. When Should You Start HIV Treatment? Treatment guidelines from the U.S. Department of Health and Human Services recommend that a person living with HIV begin ART as soon as possible after diagnosis. Starting ART slows the progression of HIV and can keep you healthy for many years. If you delay treatment, the virus will continue to harm your immune system and put you at higher risk for developing opportunistic infections that can be life threatening. Does ART Cause Side Effects? Like most medicines, antiretroviral therapy (ART) can cause side effects. However, not everyone experiences side effects from ART. The HIV medications used today have fewer side effects, fewer people experience them, and they are less severe than in the past. Side effects can differ for each type of ART medicine and from person to person. Some side effects can occur once you start a medicine and may only last a few days or weeks. Other side effects can start later and last longer. If you experience side effects that are severe or make you want to stop taking your HIV medication, talk to your health care provider or pharmacist before you miss any doses or stop taking the medication. Skipping doses or starting and stopping medication can lead to drug resistance, which can harm your health and limit your future treatment options. Some side effects of ART that are most commonly reported include:
And be aware; HIV medicines also may cause different side effects in women than men. Contact your health care provider or pharmacist immediately if you begin to experience problems or if your treatment makes you sick. If side effects make you want to skip taking your medications sometimes or stop taking them altogether, talk to your health care provider or pharmacist right away to find solutions that work for you. Your health care provider may prescribe medicines to reduce or eliminate side effects or may recommend changing your medication to another type of ART that might work better for you. Learn more about the possible side effects of ART and ways to manage them. What Is HIV Drug Resistance? Drug resistance can be a cause of treatment failure for people living with HIV. As HIV multiplies in the body, it sometimes mutates (changes form) and produces variations of itself. Variations of HIV that develop while a person is taking ART can lead to drug-resistant strains of HIV. With drug resistance, HIV medicines that previously controlled a person's HIV are not effective against new, drug-resistant HIV. In other words, the HIV medicines can't prevent the drug-resistant HIV from multiplying. Drug resistance can cause HIV treatment to fail. A person can initially be infected with drug-resistant HIV or develop drug-resistant HIV after starting HIV medicines. Drug-resistant HIV also can spread from person to person. Drug-resistance testing identifies which, if any, HIV medicines won't be effective against your specific strain of HIV. Drug-resistance testing results help determine which HIV medicines to include in an HIV treatment regimen. Taking HIV medication every day, exactly as prescribed helps prevent drug resistance. Read more about drug resistance in this fact sheet from AIDSinfo. Content Source: HIV.gov Date last updated: March 29, 2019 2. Taking Your HIV Medication Every DayWhy Should You Take Your HIV Medication Every Day?
Taking your HIV medication daily as prescribed provides many benefits. Among them, it:
Learn more: Read our fact sheet about the health and prevention benefits of viral suppression and maintaining an undetectable viral load (PDF 166 KB). Taking your HIV medication daily is also important because skipping doses makes it easier for HIV to change form, causing your medication to stop working. This is called drug resistance. HIV can become resistant to your medication and to similar medications that you have not yet taken. This limits your options for successful HIV treatment. Drug-resistant strains of HIV can be transmitted to others, too. What Should You Do If You Miss a Dose? Taking your HIV medication every day, exactly the way your health care provider tells you to will help keep your viral load low and your CD4 cell count high. If you skip doses, even now and then, you are giving HIV the chance to multiply rapidly. This could weaken your immune system, and you could become sick. Talk to your health care provider if you miss a dose. In most cases, if you realize you missed a dose, take the medicines as soon as you can, then take the next dose at your usual scheduled time (unless your pharmacist or health care provider has told you something different). If you find you miss a lot of doses, talk to your health care provider or pharmacist about ways to help you remember your medicines. You and your health care provider may even decide to change your treatment regimen to fit your health care needs and life situation, which may change over time. Do You Have to Take Your HIV Medication If Your Viral Load Is Undetectable? Yes, antiretroviral therapy (ART) reduces your viral load, ideally to an undetectable level. If your viral load goes down after starting ART, then the treatment is working, and you should continue to take your medicine as prescribed. If you keep an undetectable viral load, you can stay healthy and have effectively no risk of transmitting HIV to an HIV-negative partner through sex. Content Source: HIV.gov Date last updated: January 09, 2019 3. Tips on Taking Your HIV Medication Every Day What Are Some Tips to Help Me Take My HIV Medication Every Day?
If you're newly diagnosed with HIV, you may be seeking tips and tools to help you keep up with your HIV treatment. That's because HIV treatment involves taking HIV medication every day, exactly as prescribed to lower the amount of HIV in your body (also called the viral load) to a very low level. This is called viral suppression. If the viral load is so low that it doesn't show up in a standard lab test, this is called having an undetectable viral load. Getting and keeping an undetectable viral load is the best thing you can do to stay healthy. There is also a prevention benefit: people living with HIV who take HIV medication daily as prescribed and get and keep an undetectable viral load have effectively no risk of transmitting HIV to an HIV-negative partner through sex. Viral Suppression and Undetectable Viral Load: What Do They Mean? If taken as directed, HIV medication can reduce the amount of HIV in the blood (also called the viral load) to a very low level. This is called viral suppression. Viral suppression helps to keep you healthy and prevents illness. If the viral load is so low that it doesn't show up in a standard lab test, this is called having an undetectable viral load. How Do You Get Your Viral Load to Undetectable and Keep It There? People living with HIV can get and keep an undetectable viral load by taking HIV medication (called antiretroviral therapy or ART) every day, exactly as prescribed. Almost everyone who takes HIV medication daily as prescribed can achieve an undetectable viral load, usually within 6 months after starting treatment. But HIV is still in the body when the viral load is suppressed, even when it is undetectable. If a person stops taking HIV medication, the viral load will quickly go back up. People who have stopped taking their medication or who are having trouble taking all doses as prescribed should talk to their health care provider as soon as possible about how to get back on track. Benefits There are important health benefits to having a suppressed or undetectable viral load. People living with HIV who know their status, take HIV medication daily as prescribed, and get and keep an undetectable viral load can live long and healthy lives. There is also a major prevention benefit. People living with HIV who take HIV medication daily as prescribed and get and keep an undetectable viral load have effectively no risk of sexually transmitting HIV to their HIV-negative partners. This is often called "treatment as prevention." Also, if a woman living with HIV takes HIV medication as prescribed throughout pregnancy, labor, and delivery, and if HIV medicine is given to her baby for 4-6 weeks after delivery, the risk of transmission from pregnancy, labor, and delivery can be reduced to 1 percent or less. Talk with Your Health Care Provider Talk with your health care provider about these benefits of HIV treatment and discuss which HIV medication is right for you. Stay in medical care so your provider can regularly monitor your viral load and make sure it remains undetectable. Also talk to your provider about ways to prevent other sexually transmitted infections (STls). Having an undetectable viral load only prevents transmission of HIV, not other STls. Here are some tips that may help you take every dose of your HIV medication, every day:
4. Paying for HIV Care and TreatmentPaying for HIV Care
IV care and treatment involves taking antiretroviral therapy (ART) and having regular check-ups with your healthcare provider who will monitor your health status on an ongoing basis. These things are important because with the proper care and treatment, you can reduce your viral load, protect your health, enjoy a long and healthy life, and reduce the potential of transmitting the virus to others. But you might have concerns about how to pay for this. There are resources that can help you pay for the care you need. Private Insurance Job-Based and Individual Insurance—Many people have private health insurance through their employer (or a family member's employer), or they have individual insurance they have purchased. Under the Affordable Care Act (ACA), most job-based and individual plans are required to offer new benefits and protections. For example, plans can't can drop you or deny you coverage just because you have a pre-existing health condition, like HIV. And insurers can't impose lifetime caps on your insurance benefits. However, you'll still need to pay any deductibles, copayments, and coinsurance your plan requires. Make sure you read your plan carefully so that you know what your plan will (and won't) cover. When you leave a job, you may be able to keep your job-based health insurance for a period, usually up to 18 months. This is called COBRA continuation coverage. With COBRA coverage, you usually have to pay the entire monthly premium yourself, plus a small administrative fee. Your former employer no longer pays any of your insurance costs. The Health Insurance Marketplace—Established under the ACA, the Health Insurance Marketplace helps uninsured people find and apply for quality, affordable health coverage. Private plans in the Marketplace are required to cover a set of essential health benefits. And, low and middle-income people may qualify for lower costs, based on their household size and income. To see if you can enroll in a health insurance plan or change plans, visit healthcare.gov or find local help. Federal Resources If you do not have private health insurance—or you need help because your insurance doesn't pay for the HIV care and treatment you need—there are Federal resources that may help you. Getting Help—Figuring out which programs and services you qualify for can be confusing. But don't worry! There are case managers and benefits counselors who can help you. They know what services are available and can help you get care. Their services are free. You can find one near you by contacting a local HIV/AIDS service organization. Toll-free State HIV/AIDS Hotlines will help put you in touch with agencies that can determine what programs and services you may be eligible for and help you access them. Here are Federal resources that are available:
Non-Federal Resources Patient Assistance Programs (PAPs) are programs administered by pharmaceutical companies to offer free or reduced-cost antiretroviral (ARV) medicines to low-income people living with HIV who are uninsured or underinsured, and who do not qualify for assistance programs such as Medicaid, Medicare, or AIDS Drug Assistance Programs. Each pharmaceutical company has different eligibility criteria for qualifying for their PAP. The U.S. Department of Health and Human Services, seven pharmaceutical companies, the National Alliance of State and Territorial AIDS Directors (NASTAD), and community stakeholders worked together to develop a common patient assistance program application (CPAPA) and companion document that can be used by patients and providers to access these programs. Content Source: HIV.gov Date last updated: October 10, 2019 C. Other Related Health Issues1. Other Health Issues of Special Concern for People Living with HIVDo People Living with HIV Have Other Health Conditions?
Yes. It's common for people living with HIV to have other health issues. Some of these issues may be directly related to HIV or its treatment. Others may be completely unrelated. These health conditions can mean more doctors' visits, lab tests, and medications to keep up with. Taking HIV medication (called antiretroviral therapy or ART) daily as prescribed, and staying in regular medical care is the best way for people living with HIV to stay healthy. Pre-Existing Conditions Related to HIV Risk Sometimes people living with HIV have pre-existing conditions that may have contributed to their risk for HIV infection. These conditions can sometimes complicate HIV treatment if not addressed. Among these conditions are mental health issues, alcohol use, and drug use. The risk of HIV infection is higher among people whose lives are affected by mental health issues like depression, anxiety, or the psychological effects of bullying, sexual abuse, or physical abuse. Alcohol and drug use also increase a person's risk of exposure to HIV and other sexually transmitted diseases. Regardless of whether they played a role in someone's risk for getting HIV, mental health and substance use disorders can make it harder for people living with HIV to take ART daily as prescribed. But behavioral health treatment and services are available. Talk openly and honestly with your health care provider about your mental health and substance use so that he or she can evaluate you and help you find the support you need. Use SAMHSA's Behavioral Health Treatment Locator to find mental health and substance abuse treatment facilities near you. Common Coinfections Coinfection is when a person has two or more infections at the same time. There are some common coinfections that affect people living with HIV. For example:
Other Health Conditions Associated with HIV Thanks to improvements in HIV treatment, people living with HIV are living longer than ever. But even when HIV is well controlled with medication, it causes chronic inflammation. Over time, that takes a toll on the body, putting people living with HIV at greater risk for health conditions such as cardiovascular disease, kidney disease, diabetes, bone disease, liver disease, cognitive disorders, and some types of cancer. Your health care provider will work with you, or may refer you to a specialist, to treat any of these conditions you may develop. Some people also experience side effects from HIV medicines that can continue for a long time. See your health care provider regularly and discuss any side effects you experience. Never cut down, skip, or stop taking your HIV medications unless your health care provider tells you to. Your provider will work with you to develop a plan to manage the side effects, or may recommend that you change medication. Be sure to take care of your emotional wellness, eat a healthy diet, exercise, and quit smoking. These all play an important role in living healthy with HIV. Content Source: HIV.gov Date last updated: May 01, 2019 2. Alcohol and Drug UseAlcohol and drug use can be harmful to your health and get out of hand for some people. Modest use of alcohol can help your heart health in some circumstances, but it can also lead to long-term effects that are harmful and reduce your ability to fight off HIV. Different drugs have different effects on the body, and they can affect your judgement, mental health, and physical health differently. The use of illegal drugs presents multiple risks to the health of people living with HIV including harmful effects on the body and the risks associated with injection drug use, and risks associated with sexual transmission of HIV.
How Can Alcohol, Drug Use, and HIV Affect Your Health? Alcohol and drug use, abuse, and dependence may damage your body and brain, and drug overdoses can cause death. This damage to your body and brain can negatively affect your health and well-being in many ways. These are just some examples.
How Can You Find Treatment or Support Programs? Choosing to stop using drugs or alcohol is not easy, but it can be done. Quitting will improve your health, well-being, and relationships with others.
Support is available. Many organizations provide hotlines and guidance on substance abuse treatment options:
CDC offers more information on substance abuse and treatment. Content Source: CDC's HIV Basics Date last updated: May 15, 2017 3. Hepatitis B & CHIV and Hepatitis B and Hepatitis C Coinfection
About 1 in 10 people living with HIV are coinfected with hepatitis B virus (HBV), and about 1 in 4 people are coinfected with hepatitis C virus (HCV). Hepatitis B and C are liver infections caused by a virus. Because these infections can be spread in the same ways as HIV, people with HIV in the United States are often also affected by chronic viral hepatitis. Viral hepatitis progresses faster and causes more liver-related health problems among people with HIV than among those who do not have HIV. Liver disease, much of which is related to HBV or HCV, is a major cause of non-AIDS-related deaths among people living with HIV. Given the risks of hepatitis B or hepatitis C coinfection to the health of people living with HIV, it is important to understand these risks, take steps to prevent infection, know your status, and, if necessary, get medical care from someone who is experienced in treating people who are coinfected with HIV and HBV, or HIV and HCV. How Are Hepatitis B and C Spread from Person to Person? Like HIV, the hepatitis B and C viruses spread:
Is Hepatitis Testing Recommended for People with HIV? 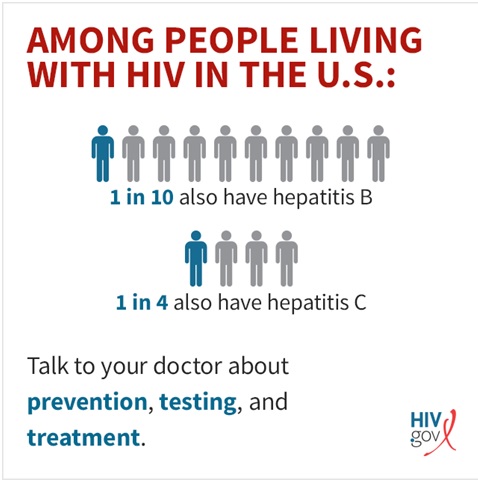 Yes. Everyone living with HIV should be tested for HBV and HCV when they are first diagnosed with HIV and begin treatment. People living with HIV who have ongoing risk factors for getting hepatitis B or C should be tested annually. How Can You Prevent Hepatitis B and C? Hepatitis B: Vaccination is the best way to prevent all of the ways that hepatitis B is transmitted. People with HIV who do not have active HBV infection should be vaccinated against it. Hepatitis C: No vaccine exists for HCV. The best way to prevent hepatitis C infection is to never inject drugs or to stop injecting drugs by getting into and staying in drug treatment. If you continue injecting drugs, always use new, sterile needles or syringes, and never reuse or share needles or syringes, water, or other drug preparation equipment. Treatment for HIV-Hepatitis Coinfection HIV-HBV and HIV-HCV coinfections can be effectively treated in most people. But treatment can be complex, and people with coinfection should look for health care providers with expertise in the management of both HIV infection and viral hepatitis. Hepatitis B: For hepatitis B, treatment can delay or limit liver damage by suppressing the virus. Like treatment for HIV, hepatitis B treatment may need to be taken for the rest of your life. Hepatitis C: New treatments for hepatitis C have been approved in recent years. These direct-acting treatments are much better than the previously available treatment because they have few side effects and do not need to be injected. These treatments for HCV infection cure more than 90% of people, including those living with HIV, in 12-24 weeks. Content Source: HIV.gov Date last updated: April 30, 2019 4. Immunizations Recommended for People Living With HIVWhat Are Immunizations?
Immunizations (also called “vaccines”) protect people from diseases such as chicken pox, flu, and polio. Vaccines are given by needle injection (a shot), by mouth, or sprayed into the nose. Most vaccines are designed to prevent a person from ever having a disease or so that a person will only have a mild case of the disease. When a person gets a vaccine, his or her body responds by mounting an immune system response to defend the body against the infection. Since HIV can make it difficult for your immune system to fight infections, people living with HIV could benefit greatly from vaccines against preventable infections. Also, vaccines don't just protect individuals from disease. They also protect communities. When most people in a community get immunized against a disease, there is little chance of a disease outbreak. Which Vaccines are Recommended for People Living with HIV? The following vaccines are recommended for people living with HIV:
Additional vaccines may be recommended based on an HIV-infected person's age, previous vaccinations, risk factors for a particular disease, or certain HIV-related factors. Talk to your health care provider about which vaccines are recommended for you. For more details, read this information from the Centers for Disease Control and Prevention (CDC): HIV Infection and Adult Vaccination. Are All Types of Vaccines Safe for People Living with HIV? There are two basic types of vaccines:
In general, to be safe, people with HIV should get inactivated vaccines to avoid even the remote chance of getting a disease from a live, attenuated vaccine. However, for some diseases, only live, attenuated vaccines are available. In this case, the protection offered by the live vaccine may outweigh the risks. Vaccines against chicken pox and shingles are examples of live, attenuated vaccines that, in certain situations, may be recommended for people with HIV. Talk to your health care provider about what is recommended for you. Can HIV Affect How Well a Vaccine Works? Yes. HIV can weaken your body's immune response to a vaccine, making the vaccine less effective. In general, vaccines work best when your CD4 count is above 200 copies/mm3. Also, by stimulating your immune system, vaccines may cause your HIV viral load to increase temporarily. Because HIV medicines strengthen the immune system and reduce HIV viral load, people living with HIV may want to start antiretroviral therapy (ART) before getting vaccinated whenever possible. In some situations, however, immunizations should be given even if ART has not been started. For example, it's important for people with HIV to get vaccinated against the flu at the time of year when the risk of flu is greatest. Talk to your health care provider about what is recommended for you. Do Vaccines Cause Side Effects? Any vaccine can cause side effects. Side effects from vaccines are generally minor (for example, soreness at the location of an injection or a low-grade fever) and go away within a few days. Severe reactions to vaccines are rare. Before getting a vaccine, talk to your health care provider about the benefits and risks of the vaccine and possible side effects. Learn about vaccine safety and possible side effects. What About Travel and Vaccines? You should be up to date on routine vaccinations, no matter where you are going. If you are planning a trip outside the United States, you may need immunizations against diseases that are present in other parts of the world, such as cholera or yellow fever. If you have HIV, talk to your health care provider about any vaccines you may need before you travel. He or she will know which vaccines are safe for you. Keep in mind:
Is There a Vaccine Against HIV? No. There is currently no vaccine that has been approved by the FDA to prevent HIV infection or treat those who have it. However, scientists are working to develop one. Learn about HIV vaccine research. Content Source: AIDS Info Date last updated: May 15, 2017 5. Mental HealthMental Health and HIV
Almost every person faces mental health challenges at some point. Major stresses—like the death of a loved one, divorce, loss of a job, or moving—can have a major impact on mental health. Having a serious illness, like HIV, can be another source of major stress. You may find that a diagnosis of HIV challenges your sense of well-being or complicates existing mental health conditions. HIV and some opportunistic infections can also affect your nervous system and can lead to changes in your behavior. Good mental health will help you live your life to the fullest and is essential to successfully treating HIV. To help manage your mental health, it is important to know when, how, and where to get help. Many mental health conditions are treatable and many people with mental health conditions recover completely. One of the most common mental health conditions that people living with HIV face is depression. Depression can range from mild to severe, and the symptoms of depression can affect your day-to-day life. Both HIV-related medical conditions and HIV medications can contribute to depression. Symptoms can include:
Other mental health conditions include anxiety disorders, mood disorders, and personality disorders. For a good deblockedion of specific mental health conditions and their symptoms, visit .mentalhealth.gov Getting help in a crisis. At times, the problems of life can take a toll on people. Some might feel trapped, hopeless, or might wonder what they have to live for. If you are having thoughts like these or are thinking about hurting or killing yourself, know that you are not alone and that things can change. SAMHSA's Suicide Prevention Lifeline provides 24/7, free and confidential support for people in distress. Get information online or call:(800) 273-TALK (8255). You can also:
Talk to Your HIV Health Care Provider Talk to your HIV health care provider if you are experiencing any of the symptoms above. Your provider may ask you some questions to assess how you are feeling and may prescribe medications to help with depression or anxiety or refer you to a mental health specialist. If you are taking antiretroviral therapy (ART) or plan to take ART, consider the following:
Communicate openly and honestly with your health care provider about your mental health so that he or she can help you find the support you need. Discuss any changes in the way you are thinking, or how you are feeling about yourself and life in general. Mental Health Providers and Programs Because mental health conditions are common, many outlets can help you maintain good mental health. If you are having symptoms of depression or another mental health condition, talk to your health care provider, social worker, or case manager. These people can refer you to a mental health provider who can give you the care you need. Types of mental health providers include:
You may also choose to join a support group. Support groups include:
Work with a trained mental health professional to learn about treatment options such as therapy and/or medicine. You and your provider can develop a plan that will help you regain and maintain good mental health. Other ways to help improve mental health and well-being include:
You may find it helpful to create an action plan for your mental well-being. SAMHSA offers a free self-help guide you can use to create and maintain a wellness plan for yourself. Find Mental Health Services Many organizations have websites and telephone hotlines that can help you find treatment for mental health conditions.
Content Source: HIV.gov Date last updated: May 08, 2018 6. Opportunistic InfectionsWhat Are Opportunistic Infections?
Opportunistic infections (OIs) are infections that occur more frequently and are more severe in people with weakened immune systems, including people with HIV. Many OIs are considered AIDS-defining conditions. That means if a person with HIV has one of these conditions, they are diagnosed with AIDS, the most serious stage of HIV infection. When a person with HIV gets certain infections (called opportunistic infections, or OIs) or specific cancers, they will get diagnosed with AIDS (also known as HIV Stage 3), the most serious stage of HIV infection. AIDS is also diagnosed if a person's CD4 cells falls below a certain level. What are Some of the Most Common Opportunistic Infections? Some of the most common OIs in people living with HIV in the U.S. are:
A more detailed list found at the CDC https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html includes:
What Causes Opportunistic Infections? OIs are caused by a variety of germs (viruses, bacteria, fungi, and parasites). These germs spread in different ways, such as in the air, in body fluids, or in contaminated food or water. They can cause health problems when a person's immune system is weakened by HIV disease. Who Is at Risk for Opportunistic Infections? People living with HIV are at greatest risk for OIs when their CD4 count falls below 200. However, some OIs can occur when a person's CD4 count is below 500. That's because weakened immune system makes it harder for the body to fight off HIV-related OIs. Are Opportunistic Infections Common in People with HIV? OIs are less common now than in the early days of HIV and AIDS when there was no treatment. Today's HIV medicines (called antiretroviral therapy or ART) reduce the amount of HIV in a person's body and keep the immune system stronger and better able to fight off infections. However, some people with HIV still develop OIs for reasons such as:
How Can You Prevent Getting Opportunistic Infections?  The best way to prevent OIs is to take HIV medication daily as prescribed so that you can get and keep an undetectable viral load and keep your immune system strong. It is also important to stay in HIV medical care and get lab tests done. This will allow you and your health care provider to know when you might be at risk for OIs and discuss ways to prevent them. Some of the ways people living with HIV can reduce their risk of getting an OI include:
Can Opportunistic Infections Be Treated? If you develop an OI, there are treatments available such as antiviral, antibiotic, and antifungal drugs. The type of medicine used depends on the OI. Once an OI is successfully treated, a person may continue to use the same medicine or an additional medicine to prevent the OI from coming back. Having an OI may be a very serious medical situation and its treatment can be challenging. For more information about specific OIs, visit CDC's Opportunistic Infections. Content Source: HIV.gov Date last updated: July 16, 2019 7. Sexually Transmitted DiseasesWhat Do You Need to Know About STDs?
Living healthy with HIV includes preventing other sexually transmitted diseases (STDs). An STD is an infection that's passed from person to person through sexual contact. HIV is an example of an STD. Other types of STDs include:
The only way to avoid getting other STDs is to not have vaginal, anal, or oral sex. If you are sexually active, you can do the following things to lower your chances of getting other STDs:
For people living with HIV, it can be harder to treat STDs. STDs increase your viral load in your genital fluids, and some types of STDs can lower your CD4 count. Because HIV weakens the CD4 cells in the immune system, your body has a harder time fighting off STDs. This also means that if you are living with HIV and also have an STD, you may be able to transmit HIV to your partner(s) even if your viral load is undetectable. In fact, people living HIV who are also infected with another STD are 3 to 5 times as likely as others living with HIV to spread HIV through sexual contact. Also, some sexually transmitted diseases affect women living with HIV differently than they affect women who do not have HIV. Learn more about these differences. It's important for people with HIV to get tested and treated for other STDs. Being tested and treated for STDs helps you maintain good health and avoid transmitting an STD unknowingly. If you have HIV and are sexually active, get tested at least once a year. Encourage your partner(s) to do the same. You or your partner(s) can have an STD without having symptoms. You and your partner should determine what sexual behaviors and prevention practices are going to be used in your relationship—and outside of it if you are not exclusive. The goal of this communication is to keep you BOTH healthy and free from new infections. Your health care provider can offer you the best care if you discuss your sexual history openly. 8. SmokingHow Does Smoking Affect People Living with HIV?
Smoking is dangerous for everyone—it is the leading cause of preventable death in the U.S. But the risks of serious health consequences are much higher for people living with HIV, who smoke at a rate 2 to 3 times greater than the general population. 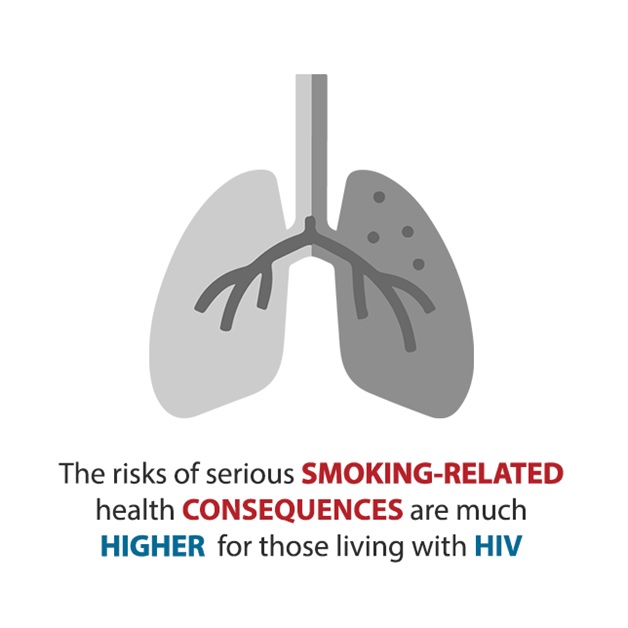 Smoking has many negative health effects on people living with HIV. For example, smokers living with HIV are more likely than nonsmokers with HIV to:
What Are the Health Benefits of Quitting? Quitting smoking has major and immediate health benefits for tobacco users, including people living with HIV. These benefits include:
You are never too old to quit. Find Help to Quit Smoking Talk with your health care provider about programs and products that can help you quit smoking. You also can learn about the benefits of quitting smoking and get tips for quitting from CDC's national tobacco education campaign—Tips From Former Smokers (Tips). The Tips campaign profiles real people—not actors—who are living with serious long-term health effects from smoking and secondhand smoke exposure. You can also view a story and tips from a person living with HIV who quit smoking. Visit betobaccofree.hhs.gov or call the Smoking Quitline: 877-44U-QUIT (877-448-7848) for more information on the many health benefits of quitting smoking. For help from your state quitline, call 1-800-QUIT-NOW (1-800-784-8669). Content Source: HIV.gov Date last updated: November 08, 2018 9. Women's Health IssuesHow Does HIV Affect Women Differently?
HIV may cause some health problems that are unique to women, such as:
Pregnancy and birth control also require careful management with a health care provider. The good news is that women who take HIV medicine (called antiretroviral therapy or ART) daily as prescribed and get and keep an undetectable viral load can stay healthy and have effectively no risk of transmitting HIV to an HIV-negative partner through sex. Gynecological Health Issues and HIV Gynecological problems are common among women living with HIV. Some of the issues women may experience are:
Treatment is available for these health conditions. Talk to your health care team about treatment options that are right for you. Cervical Cancer and HIV Women with HIV have a higher risk of cervical cancer. It is important that they be screened regularly for this disease. Cervical cancer is cancer that starts in the cervix, the lower, narrow part of the uterus (the womb). It is almost always caused by human papillomavirus (HPV) infection. The types of HPV that cause cervical cancer are more common in women with HIV. For this reason, women with HIV need to get regular Pap tests to help find changing cervical cells before they turn into cancer. Talk to your health care provider about the Pap test schedule that is right for you. In addition, the HPV vaccine is recommended for women (and men) with HIV infection through age 26. Cervical cancer is an AIDS-defining cancer. That means that a diagnosis of cervical cancer marks the point at which a person's HIV infection has progressed to AIDS. HIV Medicine Side Effects and Drug Interactions HIV medicine works as well for women as it does for men. However, some medicines can cause different side effects in women than men. For example:
In addition, HIV medicines can interact with other drugs, which can harm you or make your HIV medicines less effective. These include:
If you are taking HIV medicines and have problems with any side effects or questions about drug interactions, talk to your health care provider or pharmacist to find solutions that work for you. Do NOT cut down on, skip, or stop taking your HIV medicines unless your provider tells you to. Women's Aging and HIV Thanks to effective HIV treatment, women with HIV are living longer lives. That also means that as they age, they face the same health problems that many other older women do, such as heart disease, diabetes, high blood pressure, arthritis, and some cancers. Women with HIV also may face also other health concerns as they age. These include:
If you have questions about symptoms of the menopause or about osteoporosis, talk to your health care team. Heart Disease and HIV HIV-related heart disease is a leading cause of death among people living with HIV—even when they are on consistent, effective HIV treatment. The risk of heart attack is especially a concern for women. Women living with HIV are three times more likely to have a heart attack than women without HIV. Research is underway to learn how factors unique to women with HIV affect heart disease risk and what to do about it. Pregnancy and HIV Women with HIV can have healthy pregnancies. But some may need to switch HIV medications. Talk with your provider if you are thinking of planning a pregnancy, including about how to prevent transmission if your partner is HIV-negative. In addition, women with HIV can pass the virus to their baby during pregnancy, childbirth, or breastfeeding. The good news is that there are ways to lower the risk of passing HIV to your unborn baby to 1% or less. Birth Control and HIV Women with HIV can safely use any form of birth control to prevent pregnancy. But some HIV medicines can interact with hormonal birth control, including the shot, pills, or implants. This can raise the risk for pregnancy. Talk to your health care provider about which form of birth control is right for you. Also, using condoms the right way every time you have sex can help reduce your risk of getting STDs such as gonorrhea and syphilis.  Content Source: HIV.gov Date last updated: May 23, 2019 ----------------------------------------------------------------------------------------------------------------------- [ QN.No.#21. Treatment guidelines from the U.S. Department of Health and Human Services recommend that a person living with HIV begin ART, antiretroviral therapy, _________. a) after you have your medical team in place and have told your friends and family b) when you start showing symptoms associated with AIDS c) when you have received approval from your insurance company and have your finances in order d) as soon as possible after the diagnosis] [ QN.No.#22. Tips that may help a person take every dose of their HIV medication every day include: a) creating a routine, setting an alarm b) trying a weekly or monthly pill box c) keeping a daily log or using a calendar to keep track d) all of the above] [ QN.No.#23. One of the most common mental health conditions that people living with HIV face is ________. a) depression b) social anxiety c) bipolar disorder d) dissociative disorder] [ QN.No.#24. Some of the most common OIs, opportunistic infections, in people living with HIV in the U.S. are all of the following except: a) Lime disease b) Herpes simplex virus 1 (HSV-1) infection c) Salmonella infection d) Candidiasis (thrush) [ QN.No.#25. OIs are less common now than in the early days of HIV and AIDS when there was no treatment. Today's HIV medicine (called antiretroviral therapy or ART) reduce the amount of HIV in a person's body and keep the immune system stronger. However, some people with HIV still develop OI's for all of the following reasons except: a) they do not know they have HIV and so they are not on treatment b) they know they have HIV but are not taking ART c) they were living with HIV for a long time before they were diagnosed and so have a weakened immune system d) their detectable viral load is too low and they need their viral load numbers to increase [ QN.No.#26. Some of the ways people living with HIV can reduce their risk of getting an OI include all of the following except: a) avoiding exposure to contaminated water and food b) taking medicines to prevent certain OIs c) getting vaccinated against some preventable infections d) stop getting lab tests done so frequently to keep an undetectable viral load [ QN.No.#27. People living with HIV who are also infected with another STD are ______ likely as others living with HIV to spread HIV through sexual contact. a) less b) the same amount as c) 3 to 5 times as d) 10 times as] [ QN.No.#28. Gynecological problems are common among women living with HIV. Some of the issues women may experience include all of the following except: a) problems related to sexually transmitted diseases, like genital herpes, pelvic inflammatory disease and chancroid can occur more often b) trichinosis can occur more often with a periapical abscess c) vaginal yeast infections can occur more often and may be harder to treat d) bacterial vaginosis can occur more often and may be harder to treat] |
|
||||||||||||||||||||||||||||||||||||||||
|
HIV / AIDS Course > Chapter 6 - Staying in HIV Care
Page Last Modified On:
Deprecated: Function strftime() is deprecated in /home/devxspeedy/public_html/lib/smarty-3.1.34/libs/plugins/modifier.date_format.php on line 81 December 30, 2019, 11:59 AM |
|||||||||||||||||||||||||||||||||||||||||
